The Connection Between Alzheimer's Disease and Vision Loss
Understanding Alzheimer's Disease and Vision Loss
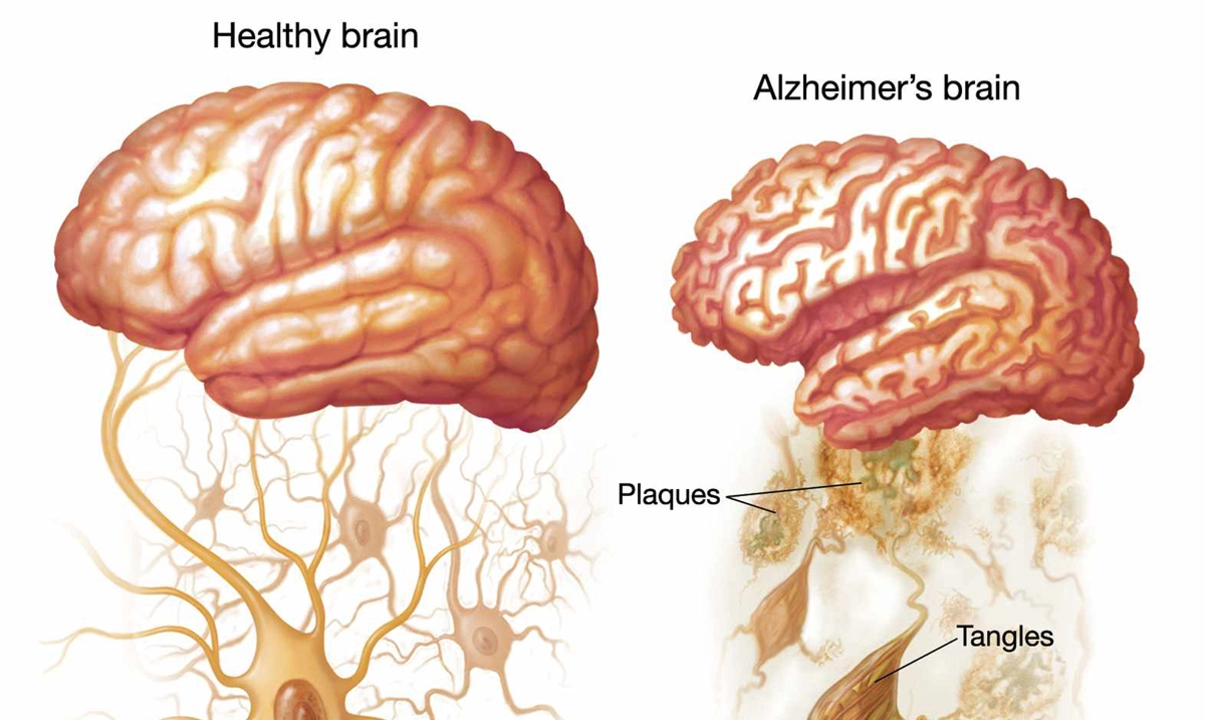
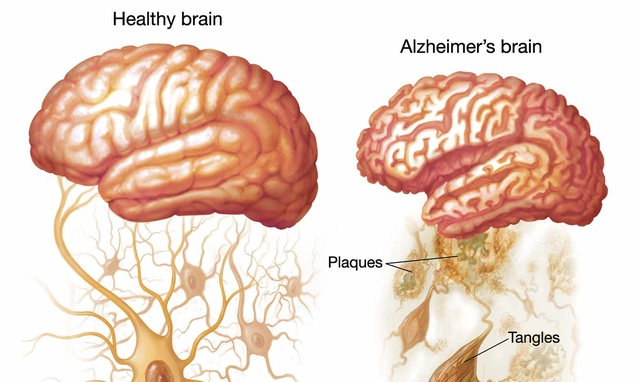
Alzheimer's Disease is a progressive, neurodegenerative condition that affects millions of people worldwide. It is characterized by the gradual decline in cognitive abilities, leading to memory loss, confusion, and eventually, the inability to perform daily tasks. One of the lesser-known symptoms of Alzheimer's Disease is vision loss. In this article, we will explore the connection between Alzheimer's Disease and vision loss, and how these two conditions are linked.
The Impact of Alzheimer's Disease on the Visual System
As Alzheimer's Disease progresses, it can have a significant impact on an individual's visual system. The brain plays a crucial role in processing visual information, and as the disease progresses, it can lead to deterioration in the visual processing areas of the brain. This can result in a range of visual disturbances, including difficulty recognizing faces, objects, or even perceiving depth and distance accurately.
Additionally, Alzheimer's Disease can cause damage to the nerve cells responsible for transmitting visual information from the eyes to the brain. This can lead to a decline in visual acuity and contrast sensitivity - making it difficult for individuals to see fine details or distinguish between different shades of light and dark.
Common Vision Problems Associated with Alzheimer's Disease
There are several vision problems that are commonly associated with Alzheimer's Disease. These include:
1. Reduced Visual Acuity
As mentioned earlier, the damage caused by Alzheimer's Disease to the nerve cells responsible for transmitting visual information can result in reduced visual acuity. This means that individuals with Alzheimer's may have difficulty seeing fine details, which can make it challenging for them to read, recognize faces, or complete daily tasks that require precise vision.
2. Contrast Sensitivity Loss
Another common vision problem associated with Alzheimer's Disease is a loss of contrast sensitivity. This makes it difficult for individuals to distinguish between different shades of light and dark, which can lead to problems with depth perception and navigating their environment safely.
3. Visual Field Defects
Visual field defects are areas of partial or complete vision loss that occur within an individual's field of view. Alzheimer's Disease can cause damage to the areas of the brain responsible for processing visual information, leading to blind spots or reduced peripheral vision. This can make it difficult for individuals to navigate their environment and increase their risk of falls and accidents.
The Role of the Eye in Alzheimer's Disease Detection
Recent research has shown that the eye could play a significant role in the early detection of Alzheimer's Disease. Studies have found that the presence of certain biomarkers in the eye, such as amyloid-beta proteins, could indicate the presence of Alzheimer's Disease in the brain. This has led to the development of non-invasive eye tests that could potentially be used to detect Alzheimer's Disease at an earlier stage, allowing for earlier intervention and potentially slowing the disease's progression.
Furthermore, monitoring changes in an individual's vision could also provide valuable information about the progression of Alzheimer's Disease. As the disease advances, it can cause significant changes in an individual's visual abilities, and monitoring these changes could help healthcare professionals track the disease's progression and adjust treatment plans accordingly.
Adapting to Vision Loss in Alzheimer's Disease
Coping with vision loss can be challenging for individuals with Alzheimer's Disease, as it can exacerbate their cognitive decline and make it more difficult to perform daily tasks. However, there are strategies that can help individuals with Alzheimer's adapt to their vision loss and maintain their independence as much as possible. These include:
1. Environmental Modifications
Making changes to an individual's living environment can help them adapt to their vision loss and reduce their risk of falls and accidents. This may involve using contrasting colors to make objects and surfaces more visible, improving lighting, and removing any hazards that could pose a risk to their safety.
2. Assistive Devices
There are a range of assistive devices available that can help individuals with Alzheimer's Disease and vision loss complete daily tasks more easily. These may include magnifying glasses, talking clocks, and large-print books.
3. Vision Rehabilitation Services
Individuals with Alzheimer's Disease and vision loss may benefit from vision rehabilitation services, which can help them develop strategies and techniques to cope with their vision loss and maintain their independence.
Support for Individuals with Alzheimer's Disease and Vision Loss
It is essential for individuals with Alzheimer's Disease and vision loss to receive the support and care they need to manage their condition effectively. This may involve working with a team of healthcare professionals, including ophthalmologists, neurologists, and occupational therapists, who can help them develop strategies to cope with their vision loss and maintain their quality of life.
Additionally, family members and caregivers can play a crucial role in supporting individuals with Alzheimer's Disease and vision loss. By understanding the challenges they face and providing a supportive, understanding environment, caregivers can help individuals with Alzheimer's Disease maintain their independence and dignity as they navigate this difficult journey.


Royberto Spencer
When we contemplate the mind's eye, it becomes evident that Alzheimer’s does not merely erode memory, it also clouds the very lenses through which we perceive the world.
The degradation of neural pathways responsible for visual integration manifests as reduced acuity and distorted depth perception.
This intertwined decline challenges our moral duty to craft environments that safeguard dignity for those afflicted.
Simple adjustments-high‑contrast fixtures, ample lighting, and uncluttered spaces-reflect a society that values its most vulnerable members.
Ignoring these needs would be a silent concession to neglect.
Annette van Dijk-Leek
Incredible how quickly research is shedding light on this hidden connection!!!
Katherine M
Esteemed colleagues, the exploration of ocular biomarkers as early indicators of neurodegeneration represents a commendable stride toward preventative medicine.😊
Integrating ophthalmic screening into routine geriatric assessments could feasibly unveil pathological changes before cognitive symptoms manifest, thereby affording precious therapeutic windows.📚
Such interdisciplinary collaboration honors both scientific rigor and the humane imperative to alleviate suffering.
Bernard Leach
The visual cortex relies on intact synaptic transmission to decode the complex patterns of light that reach our eyes.
Alzheimer's pathology disrupts these synapses through accumulation of tau tangles and amyloid plaques.
As a result, signal fidelity diminishes, leading to subtle but progressive deficits in visual acuity.
Patients may first notice difficulty distinguishing subtle shades, which can be mistaken for simple aging.
Over time, the impairment expands to include loss of contrast sensitivity, affecting everyday tasks like reading medication labels.
Moreover, the disease undermines the brain's ability to integrate visual information with memory, causing misrecognition of familiar faces.
This phenomenon, known as visual agnosia, often goes unreported because patients lack insight into their own deficits.
Clinicians should therefore incorporate systematic visual assessments into cognitive evaluations.
Simple tools such as the Pelli‑Robson chart can quantify contrast sensitivity efficiently.
In addition, retinal imaging technologies are emerging that may visualize amyloid deposition directly.
Early detection through ocular biomarkers could guide therapeutic interventions before irreversible neuronal loss occurs.
Practically, caregivers can mitigate risk by enhancing environmental lighting and using high‑contrast décor.
Assistive devices like magnifiers and talking clocks empower individuals to maintain autonomy.
Collaboration among neurologists, ophthalmologists, and occupational therapists is essential for comprehensive care.
Ultimately, acknowledging the visual dimension of Alzheimer’s enriches our understanding and improves quality of life for patients.
Shelby Larson
Honestly, the research is spot on and everyone should read this, it’s not rocket science.
The brain‑eye connection is real, and denying it is just plain ignorant.
Get your facts straight, folks.
Mark Eaton
Let’s keep pushing the boundaries of what we know-every new insight brings hope!
By sharing these findings, we empower families to adapt and thrive despite challenges.
Stay optimistic and proactive; small changes make a big difference.
Alfred Benton
While the presented data appears thorough, one must question the underlying motives of the institutions promoting ocular screening.
It is plausible that commercial interests are steering research toward profitable diagnostics rather than genuine patient benefit.
Susan Cobb
Some might argue that focusing on vision diverts attention from core cognitive therapies, yet integrating both could be more holistic.
Ivy Himnika
Dear readership, the interdisciplinary approach outlined herein exemplifies best practices in modern neuro‑ophthalmology.😊
Adhering to such protocols ensures that patients receive comprehensive evaluation, aligning clinical excellence with compassionate care.📖
Nicole Tillman
Recognizing visual impairment as a facet of Alzheimer’s does not diminish the importance of memory care; rather, it enriches our therapeutic toolbox.
By addressing both domains concurrently, clinicians can tailor interventions that respect the full spectrum of patient needs.
Sue Holten
Oh sure, because painting the walls neon orange will totally solve neurodegeneration, right? 🙄
Tammie Foote
We owe it to our loved ones to make homes safer-simple steps can prevent falls and preserve dignity.