Health and Medicine
Biologics Safety: Infection Risk, Screening, and Vaccination Guidance for Autoimmune Patients
When you’re prescribed a biologic for rheumatoid arthritis, psoriasis, or Crohn’s disease, it’s not just about managing inflammation. It’s about surviving the side effects - especially infections. Biologics are powerful. They silence parts of your immune system to stop your body from attacking itself. But that same silence makes you vulnerable. The risk isn’t theoretical. People on these drugs are 2.1 times more likely to be hospitalized for infections than those on older medications. And it’s not random. There are clear patterns, proven protocols, and life-saving steps most patients never hear about.
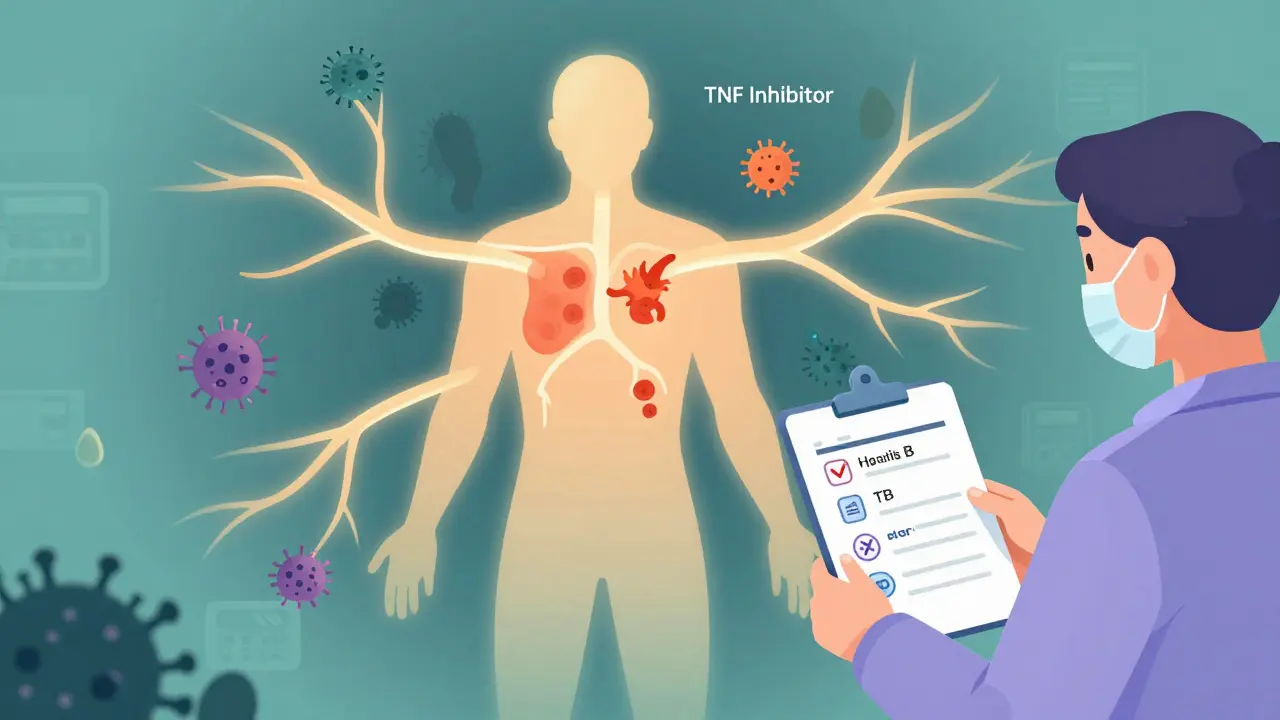
Why Biologics Increase Infection Risk
Biologics don’t weaken your immune system the way chemotherapy does. They’re more like precision tools. TNF inhibitors - drugs like adalimumab and infliximab - block a specific protein called tumor necrosis factor, which drives inflammation. But that same protein also helps your body fight off bacteria and viruses. When it’s turned off, your defenses drop. A 2019 study tracking nearly 2,000 patients found those on TNF inhibitors had a 78% higher chance of serious infections like pneumonia, tuberculosis, or sepsis compared to those on methotrexate alone. Not all biologics carry the same risk. Newer agents like ustekinumab (Stelara) and secukinumab (Cosentyx) target different pathways and show lower infection rates. In fact, one large registry study found ustekinumab users had infection rates close to those on non-biologic drugs. Certolizumab (Cimzia), which lacks a part of the antibody structure called the Fc region, has a 18% lower risk of respiratory infections than other TNF blockers. But here’s the catch: even low-risk drugs aren’t risk-free. IL-17 inhibitors like secukinumab increase the chance of candidiasis - fungal infections in the mouth or genitals. JAK inhibitors like tofacitinib, though technically not biologics, carry a 1.33x higher risk of shingles than traditional biologics.Who’s at Highest Risk?
It’s not just the drug. It’s you. Age matters. Every decade past 50 increases your infection risk by 37%. If you’re over 65, your body doesn’t respond to vaccines as well, and your immune system is already slower to react. Diabetes? That doubles your risk. Chronic kidney disease? Even worse - 2.15 times higher. COPD? You’re 2.4 times more likely to get a bad lung infection. And if you’re taking steroids - even 10mg of prednisone a day - that multiplies your infection risk by 2.3 times. The biggest silent danger? Hidden infections. Many people carry hepatitis B without knowing it. In autoimmune patients, the rate of occult (hidden) hepatitis B is 4.3%. Without screening, starting a biologic can trigger a deadly reactivation - up to 27.6% of these patients will get severe liver damage or failure. Latent tuberculosis is another hidden threat. In high-prevalence areas, up to 12.7% of patients test positive on IGRA tests. But in low-risk regions, that number may be misleading. Some experts argue routine IGRA screening leads to unnecessary treatment in places like rural Alabama, where TB cases are rare.The Three-Step Safety Protocol
There’s a proven way to avoid these dangers. It’s not complicated. It’s just rarely done right. Step 1: Screen before you start. Every patient must get three blood tests for hepatitis B: HBsAg, HBsAb, and HBcAb. If HBcAb is positive, you need a follow-up HBV DNA test. That’s how you catch the 8.7% with hidden virus. For TB, use an interferon-gamma release assay (IGRA), not the old skin test. It’s more accurate. Do this at least four weeks before your first biologic dose. Step 2: Vaccinate before you start. Live vaccines - like MMR or varicella - must be given at least four weeks before your first injection. Inactivated vaccines - flu, pneumococcal, tetanus - need two weeks. And don’t assume your childhood shots are enough. For hepatitis B, you need a blood test after your final shot to confirm you’ve built immunity (anti-HBs ≥10mIU/mL). For chickenpox, your IgG level must be above 140mIU/mL. If it’s not, you need a second round of shots. Shingrix, the shingles vaccine, is inactivated and safe to give before biologics - yet 37% of patients never get it. Step 3: Document everything. The FDA requires your screening and vaccination records to be kept for 10 years after stopping treatment. Yet in 2023, CMS audits found 23.7% of clinics didn’t comply. If you’re switching doctors, bring your own copies. Don’t rely on electronic records. They’re not always linked.What Vaccines You Need - And When
Here’s exactly what to ask for before your first biologic:- Influenza: Annual shot (not nasal spray). Get it every fall.
- Pneumococcal: Two shots - PCV20 or PCV15 first, then PPSV23 one year later. This prevents pneumonia and bloodstream infections.
- Hepatitis B: Three-dose series. Confirm immunity with blood test.
- Shingrix: Two doses, 2-6 months apart. Even if you had chickenpox or shingles before.
- MMR and Varicella: Only if you’re not immune and haven’t had them. Must be done at least four weeks before biologics.
- Tdap: One dose, then Td every 10 years.
Real Stories, Real Mistakes
One patient on Reddit shared: “My GI doctor started me on Stelara without checking my vaccines. I got shingles four months later. I was in so much pain I couldn’t sleep for weeks.” That’s not rare. A 2023 survey of over 1,200 patients found 63% had at least one screening or vaccination step skipped. The most common omissions? Not testing for hepatitis B core antibody (41%) and not checking chickenpox immunity (37%). But there are success stories. A patient in Minnesota wrote: “The clinic ran a full 12-point checklist before my Humira. They caught latent TB. I got treated for nine months. Then I started biologics. Three years later - zero infections.” That’s the difference between a rushed appointment and a system that works.
The New Rules Coming in 2025
The FDA just released draft guidance requiring drug makers to prove their biologics don’t cause more infections in real-world use - not just in clinical trials. That means future drugs will have stricter safety labels. The CDC’s updated Biosafety Guidelines (BMBL 7th Edition, due October 2025) will include new rules on how long pathogens survive in clinics and what PPE staff need when handling biologic waste. AI tools are starting to help too. The Cerner Biologics Safety Algorithm, validated in a 2023 JAMA study, uses 87 data points - from your BMI to your last flu shot - to predict your personal infection risk. It’s not perfect, but it’s better than guessing.What You Can Do Right Now
You don’t need to wait for your doctor to bring it up. Take control:- Call your pharmacy or clinic. Ask: “Did I get tested for hepatitis B and TB before starting biologics?”
- Check your vaccine records. Do you have proof of Shingrix? Hepatitis B immunity? Pneumococcal shots?
- If you’re unsure, get a blood test for HBcAb and VZV IgG. They’re cheap and covered by insurance.
- Print out the CDC’s 12-point checklist for biologic safety. Bring it to your next appointment.


Stephen Craig
It’s not the drug that kills you-it’s the silence around it. We treat biologics like magic bullets, but no one talks about the quiet erosion of immunity. We’re told to trust the science, but the science doesn’t whisper warnings-it shouts them from behind a curtain.
Vicki Yuan
Thank you for this. I’ve been on Stelara for two years and never knew I needed a VZV IgG test. My clinic skipped it-said ‘you had chickenpox as a kid, you’re fine.’ Turns out I didn’t even remember having it. Got tested last month. IgG was borderline. Got the second Shingrix shot yesterday. This should be standard.
Uzoamaka Nwankpa
I wish someone had told me this before I got hospitalized with pneumonia. I was on adalimumab. They didn’t test me for TB. I didn’t know I carried it. Now I’m on antibiotics for life. My body doesn’t feel like mine anymore.
Chris Cantey
They say ‘precision medicine.’ But what if the precision is just a marketing term for selective ignorance? They target TNF because it’s profitable to block it-not because it’s the safest path. The real danger isn’t the drug. It’s the system that profits from your vulnerability.
Terri Gladden
OMG I JUST REALIZED I NEVER GOT SHINGRIX!! I’M ON CIMZIA AND I JUST GOT A COLD AND NOW I’M SCARED I’M GONNA GET SHINGLES AND DIE IN MY SLEEP!!! I’M CALLING MY DOCTOR RIGHT NOW!!
Jennifer Glass
I appreciate how detailed this is. I’m on tofacitinib and didn’t realize JAK inhibitors carry a higher shingles risk than biologics. My doctor just said ‘you’re fine.’ I’m going back with this list. Maybe if enough of us ask, they’ll start asking too.
Joseph Snow
This is fearmongering dressed as medical advice. The FDA has approved these drugs. The CDC endorses them. The fact that you’re citing anecdotal Reddit stories and cherry-picked registry data suggests you’re not a clinician-you’re an alarmist. If you’re scared of infection, don’t take the drug. But don’t scare others into rejecting life-saving treatment based on emotional narratives.
Akshaya Gandra _ Student - EastCaryMS
i read this and i think abt my aunt she on biologics n she never got any tests i think she might hav latent tb but no one told her... i dont know if i should tell her or not
Jacob Milano
Man, this is the kind of post that makes you feel like you’re finally being spoken to like a human. Not a patient number. Not a risk category. You actually laid out the steps like someone who’s been there. I printed this. Taped it to my fridge. My wife made me a checklist with checkboxes. We’re doing this right now. Thank you.
Enrique González
Been on Humira for 4 years. Got the full screening. Got Shingrix. Got pneumococcal. Got tested for HBV. Zero infections. It’s not magic. It’s just doing the boring stuff. Most people skip it because it’s not glamorous. But your body remembers what you forget.
Aaron Mercado
Why is this not mandatory?!?!?!?!?!!? Why are doctors just... winging it?!?!?!!? I’ve seen patients die from this! I’ve seen families cry because ‘the doctor forgot’! This isn’t negligence-it’s systemic malpractice! Someone needs to sue the AMA! I’m filing a complaint with my state board right now!
saurabh singh
in india, we don’t even have access to most of these tests. my cousin is on adalimumab and they just gave her a TB skin test-no igra, no hbv dna, no nothing. she got a fungal infection last month. i showed her this post. she’s going to the private clinic next week. hope she can afford it.
Dee Humprey
You’re not alone. I was that patient who skipped the vaccine because I thought ‘I’m young, I’ll be fine.’ Got shingles at 38. It felt like my nerves were on fire. I cried for three days. Don’t wait. Get the shots. Print the checklist. Bring it. Your future self will thank you.
John Wilmerding
It is imperative to underscore that adherence to the CDC’s 12-point protocol for biologic safety is not merely a clinical recommendation-it is a standard of care. Non-compliance constitutes a breach of the duty of prudence owed to patients under the Hippocratic injunction. I encourage all practitioners to institutionalize pre-biologic screening as a mandatory workflow, not an optional addendum.
Vikram Sujay
There is a deeper question here: if we silence part of the immune system to heal the body, are we not also silencing the body’s wisdom? The body does not attack itself without reason. Perhaps the real risk is not infection-but the assumption that we can isolate inflammation from the whole. Medicine treats symptoms. Healing requires listening. This checklist saves lives. But does it heal the soul?