How to Decide When to Replace Expired OTC First-Aid Medications

Most people keep a first-aid kit at home, but how many of them actually check what’s inside? By the time an emergency happens-like a severe allergic reaction, a deep cut, or a sudden asthma attack-you don’t want to reach for a bottle that’s been sitting there for three years. Expired over-the-counter (OTC) first-aid medications aren’t just useless; some can be dangerous. Knowing when to replace expired OTC first-aid medications isn’t just good sense-it’s a safety habit that could save a life.
Not All Expired Medications Are the Same
It’s a common myth that all expired meds turn toxic or become poison. That’s not true. Most solid pills like ibuprofen, acetaminophen, or aspirin don’t suddenly turn harmful after their expiration date. Instead, they slowly lose strength. A 2019 U.S. Department of Defense study found that 80% of unopened, properly stored pain relievers still had at least 90% of their original potency-even 15 years after expiration. But that doesn’t mean you should keep them forever. The real danger comes from medications that degrade unpredictably. Liquid formulas, creams, and emergency treatments like epinephrine pens, nitroglycerine tablets, and eye drops are far more fragile. For example, epinephrine auto-injectors (EpiPens) can lose 20-30% of their potency within six months of expiration. In a life-threatening allergic reaction, that drop could mean the difference between life and death. The FDA explicitly says: never use an expired EpiPen if you have a better option. If it’s your only choice, use it anyway-but call 999 immediately after.What Needs Immediate Replacement
There are five categories of OTC first-aid items that should be tossed the moment they expire:- Epinephrine auto-injectors (EpiPen, Adrenaclick): Lose potency fast. Even if they look fine, they may not deliver a full dose.
- Nitroglycerine tablets: Used for chest pain. These tablets break down quickly once the bottle is opened-even if the date is still far off. Replace every 3-6 months after opening.
- Liquid antibiotics: Like amoxicillin suspension. Bacteria can grow in them after expiration, turning them into a health risk instead of a cure.
- Eye and ear drops: Once opened, they’re exposed to air and bacteria. Expired drops can cause serious infections.
- Rescue inhalers (albuterol): Lose effectiveness after 12 months of being removed from the foil wrapper, even if the printed date is later.
These aren’t items you can gamble with. If one of these is expired, replace it the same day. Don’t wait for your next pharmacy trip. Keep a spare EpiPen in your car, bag, or workplace.
What’s Safer to Use (Briefly) Past Expiration
If you’re out of painkillers and your ibuprofen is two months past its date, you’re probably fine. Same with antihistamines like diphenhydramine (Benadryl). A 2020 University of Florida study showed these retain about 85% effectiveness for up to 18 months past expiration, assuming they’ve been stored properly. Solid tablets in their original packaging, kept cool and dry, last longer than you think. But watch for signs of degradation:- Chalky, cracked, or discolored pills
- Medications that smell odd-like vinegar or mold
- Tablets that crumble when you touch them
If you see any of these, toss it. Even if it’s “only” a week past the date. A pill that’s physically broken down might not dissolve properly in your stomach, meaning you get no relief.
Topical Treatments Are Riskier Than You Think
Hydrocortisone cream, antibiotic ointments like Neosporin, and antiseptic gels might seem harmless-but they’re breeding grounds for bacteria after expiration. A 2023 FDA lab study found that 47% of expired hydrocortisone creams had bacterial contamination. That’s not just ineffective-it’s a direct path to a skin infection. Even antiseptics like hydrogen peroxide are time-sensitive. Once you open the bottle, it starts breaking down. After 30 days, it’s mostly water. You’re not disinfecting-you’re just rinsing. Isopropyl alcohol (70%) is more stable, but only if the bottle stays sealed. Once opened, use it within two years.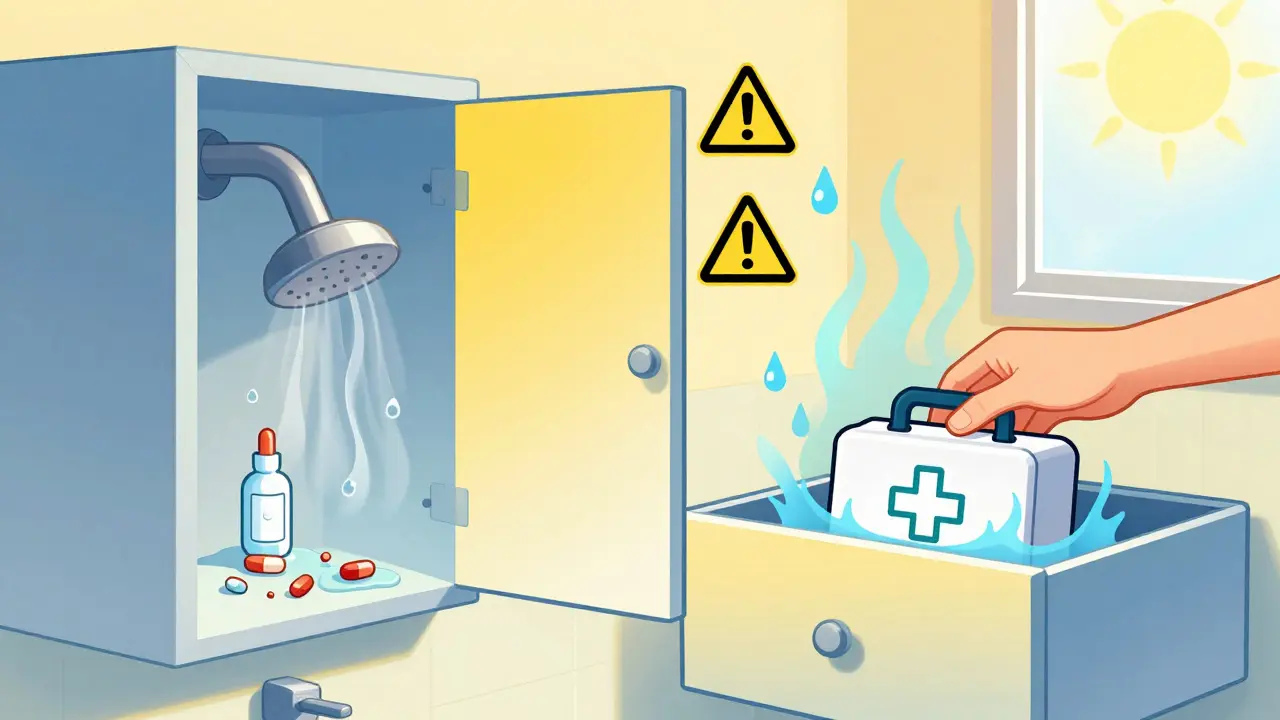
Storage Matters More Than You Realize
Your bathroom cabinet is the worst place for medications. Humidity, heat, and steam from showers speed up degradation. A 2022 Johns Hopkins study showed medications stored in bathrooms lost potency 40% faster than those kept in a cool, dry drawer. Here’s how to store them right:- Keep meds in their original bottles with the moisture-absorbing packet still inside.
- Store in a bedroom drawer, kitchen cabinet away from the stove, or a dedicated box under the sink-not in the bathroom.
- Avoid transferring pills to pill organizers unless you’re taking them daily. Once they’re out of the original packaging, their shelf life drops by 35-50%.
- Don’t leave them in the car. Summer temps can hit 60°C (140°F) inside a parked car-enough to melt pills and ruin liquids.
How to Check and Maintain Your First-Aid Kit
The American Red Cross recommends a simple four-step routine:- Check every three months: Look for changes in color, smell, texture. Are pills stuck together? Is cream watery? Toss it.
- Review expiration dates twice a year: Set a reminder on your phone for April and October. Go through every item.
- Replace emergency meds 30 days before they expire: Don’t wait until the last day. If your EpiPen expires in June, buy a new one in May.
- Do a full kit overhaul once a year: Empty everything out. Wipe down the container. Restock with new items. Throw out anything questionable.
Don’t rely on memory. Write the expiration date on the outside of the bottle with a marker if it’s faded. Or take a photo of your kit every January and compare it to the next year.
What to Do If You’re Forced to Use an Expired Medication
Sometimes, you’re stuck. You’re miles from a pharmacy. Your child has a severe reaction. Your EpiPen is expired-but it’s all you have. The Cleveland Clinic’s advice is clear: Use it anyway. A partial dose of epinephrine is better than none. A weak inhaler is better than no breathing support. But don’t stop there.- Use the expired item immediately.
- Call 999 or get to the nearest emergency room right away.
- Let medical staff know what you used and when it expired.
- Replace the item the same day.
This isn’t about being brave. It’s about survival. But it’s also about never letting it happen again.

What’s Changing in 2025
New rules are coming. Starting in December 2025, all OTC manufacturers in the U.S. must submit full stability data for every product. That means expiration dates will be more accurate and consistent. Some companies are already testing smart packaging: QR codes that scan your storage conditions and estimate remaining potency. Temperature-sensitive labels that change color if your meds got too hot are also in testing. In the UK, the NHS and pharmacy regulators are watching these developments closely. While UK laws don’t yet require smart labels, many pharmacies now offer free disposal of expired meds at drop-off points. You can also check with your local pharmacy for take-back programs.Final Rule: When in Doubt, Toss It
There’s no shame in throwing away a $10 bottle of ibuprofen. There’s huge risk in keeping it. The cost of replacing a medication is tiny compared to the cost of a hospital visit, an allergic reaction gone wrong, or a wound that turns septic. Your first-aid kit isn’t a closet full of old stuff. It’s your emergency lifeline. Treat it like one. Check it. Replace it. Keep it fresh. Because when the moment comes, you won’t have time to think-only to act. Make sure what you’re reaching for will actually work.Can I still use expired painkillers like ibuprofen or paracetamol?
Yes, but only if they’re solid tablets, still in their original sealed packaging, and stored in a cool, dry place. Studies show many retain 90%+ potency for years past expiration. But if they’re discolored, cracked, or smell odd, throw them out. Never use them for serious pain or if you’re unsure.
What should I do with expired medications?
Don’t flush them or throw them in the trash. Take them to your local pharmacy-they often have free take-back bins. In the UK, many pharmacies participate in the NHS’s medication disposal program. Some local councils also host collection days. This keeps harmful chemicals out of water systems and prevents accidental ingestion.
Is it safe to use expired antiseptic wipes or bandages?
Antiseptic wipes lose effectiveness after 2-3 years, even if unopened. The active ingredients break down, so they won’t kill germs properly. Sterile gauze and bandages can still be used if unopened and undamaged, but if the packaging is torn, moist, or discolored, throw them out. Contaminated dressings can cause infections.
Why do some meds expire so quickly after opening?
Once you open a bottle, you expose the contents to air, moisture, and bacteria. Eye drops, liquid antibiotics, and nitroglycerine tablets are especially sensitive. For example, nitroglycerine breaks down rapidly when exposed to light and air-even if the bottle is closed. That’s why pharmacists write the opening date on the label and recommend replacing them every 3-6 months.
Should I keep an expired EpiPen as a backup?
No. Never rely on an expired EpiPen as a backup. If it’s expired, replace it immediately. In a life-threatening reaction, an underdosed EpiPen might not stop the reaction-and you won’t have time to get a new one. Always carry two current, unexpired EpiPens if you’re at risk for anaphylaxis.
Next Steps for Your First-Aid Kit
Start today. Grab your first-aid kit. Lay everything out on the table. Check each item’s expiration date. Write down what’s expired. Make a list of what you need to replace. Go to your pharmacy this week. Buy new EpiPens, eye drops, and antiseptic solutions. Restock your painkillers and bandages. Clean the container. Put everything back neatly.Do this once every six months. Make it part of your routine-like checking your smoke alarms. Your future self, or someone you love, will thank you when it matters most.



Rachel Wermager
Let’s be clear: the pharmacokinetic degradation profiles of solid-dose analgesics like ibuprofen and acetaminophen are governed by Arrhenius kinetics, meaning shelf life is exponentially sensitive to thermal stress. The FDA’s Shelf Life Extension Program data confirms >90% potency retention in sealed, ambient-stored tablets beyond 15 years-provided relative humidity is <60%. But topical agents? Hydrocortisone’s degradation via hydrolysis of the ketone moiety renders it not just ineffective but pro-inflammatory. Bacterial colonization in aqueous formulations is non-negotiable. Toss it.
Storage is the silent killer. Bathroom cabinets are microbial incubators. Keep meds in desiccated, opaque containers in a 15–25°C environment. Pill organizers? Only for daily regimens. Once out of original packaging, oxidation accelerates. You’re not saving money-you’re risking organ failure.
Epinephrine auto-injectors degrade via oxidative deamination. Even if the solution looks clear, potency drops 20–30% post-expiry. That’s not a gamble. That’s negligence. Same with nitroglycerin-volatile ester, light-sensitive, loses 50% potency in 3 months post-opening. Don’t wait for the date. Track the opening date.
And yes, expired antiseptic wipes? They’re glorified wet paper towels. Hydrogen peroxide decomposes into water and oxygen. After 30 days, it’s just H₂O. Use 70% isopropyl alcohol sealed in amber glass. Replace it biannually. No excuses.
Leonard Shit
lol i just checked my first aid kit and found an epipen from 2019. i’ve been carrying it in my backpack since college. guess i’m basically a walking time bomb. also my benadryl is 4 years old but it still looks fine so… i’m gonna keep it. if i die, at least i died trying. also why is everyone so obsessed with expiration dates? i’ve eaten expired yogurt and lived. meds are just fancy yogurt.
also my bathroom cabinet is my ‘medication zen garden’. steam is nature’s humidifier. who needs science?
Brian Anaz
This whole post is liberal nonsense. You people act like expired aspirin is gonna kill you. In my day, we used whatever was in the drawer. If it worked, you kept it. If it didn’t, you went to the doctor. No one cared about dates. Now you got people replacing ibuprofen like it’s a fashion accessory. You’re not saving lives-you’re making the pharmaceutical industry rich.
And storing meds in a drawer? That’s what the rich do. I keep mine in my glovebox. If it melts, it was meant to be. America’s getting soft.
Kelly Beck
Y’ALL. I just did my first-aid kit check and it felt like a mini life reset 🌿✨
I tossed 7 expired things, bought 5 new ones (including two EpiPens-yep, I’m that person now), and even wiped down the box with a disinfectant wipe. It’s wild how much better I feel knowing my kit won’t fail me. Like, I’m not just prepared-I’m empowered. And guess what? I’m gonna do this every season now. April, July, October, January. My future self is already hugging me.
Also, I put sticky notes on everything with the expiration date. No more guessing. You’re welcome, future me. 💪❤️
Katie Schoen
so i read this whole thing and then i went to my bathroom cabinet and found a 2018 tube of Neosporin. i’ve been using it on every paper cut since 2020. honestly? it’s probably full of bacteria now. but it smells like mint and i like the ritual. also i’m pretty sure i’ve used expired eye drops before and didn’t go blind. so… maybe the real danger is overthinking this?
also why does everyone treat first aid like it’s a military operation? i just want to put a bandaid on and move on.
Beth Templeton
Expired meds aren’t dangerous unless you’re dumb enough to use them for emergencies. Ibuprofen? Fine. EpiPen? Toss it. Done.
Storage? Cool dry place. Not hard.
Stop overcomplicating it.
Dana Termini
I appreciate the depth here. I used to ignore expiration dates until my sister had a reaction and her EpiPen didn’t work. Turned out it was expired by 11 months. We got lucky. She’s fine now. But I don’t take chances anymore. I replace everything 30 days early. It’s not about being paranoid-it’s about being responsible. And honestly? It’s easier than you think. Just set a calendar reminder. You’ll thank yourself later.
Also, I keep my kit in a plastic bin under my bed. No humidity, no heat, no drama.
Isaac Jules
Everyone’s acting like this is rocket science. It’s not. You’re not a pharmacist. You’re not a scientist. You’re a human with a first-aid kit. If you’re worried about potency, don’t use it. If you’re not worried, use it. End of story.
But you people? You need a 2000-word essay on hydrolysis rates and Arrhenius equations just to decide whether to take a pill. You’re not safer-you’re just anxious.
Also, the FDA doesn’t care about your bathroom cabinet. Stop pretending they do.
Amy Le
Oh look, another American who thinks their way is the only way. In India, we’ve been using expired antibiotics for decades. People don’t die from expired ibuprofen. They die from poverty. From lack of access. From greed. You spend $50 on a new EpiPen because you’re too lazy to walk to a pharmacy? That’s not safety. That’s capitalism.
And storing meds in a drawer? In a country where 40% of homes don’t have AC? You’re not protecting your meds-you’re protecting your privilege.
Also, why is everyone so obsessed with ‘replacement’? Why not fix the system instead of buying more plastic bottles?
Pavan Vora
i am from india, and we use expired medicine all the time, because we have no choice. my father used expired paracetamol for 7 years, and he is still alive. in usa, you have so much, you even worry about the expiration date of bandage. here, we are happy if we get medicine at all. i think you should be grateful, not scared. also, i think you should not waste money on new epipen every year. use old one, and pray. 🙏
Stuart Shield
Blimey, this is the most sensible thing I’ve read on Reddit this week. Properly stored meds? Cool. Expired eye drops? Bin ‘em. EpiPen? Don’t be a hero. I once used a 10-year-old antiseptic wipe on a cut and ended up with a staph infection that took three weeks to clear. The smell? Like a gym sock dipped in vinegar. Not worth it.
My kit’s in a tin under the bed. No steam, no sun, no drama. I even write the date on the bottle with a Sharpie. Simple. Effective. And yeah-I check it every October. Like changing the smoke alarm batteries. Routine. Not neurosis.
Indra Triawan
Why do we even have expiration dates? Who decided that? Is it the corporations? The FDA? The pharmaceutical giants? They profit from our fear. They want us to keep buying. What if the real danger isn’t the expired medicine… but the system that makes us afraid to use what we already have?
I’ve kept my aspirin since 2017. It’s still in the bottle. It still looks like aspirin. Why should I pay $12 for a new one? Why do we trust labels more than our own eyes?
Maybe the medicine isn’t expired… maybe we are.
Lily Lilyy
Thank you for this thoughtful, well-researched, and deeply compassionate guide. As someone who works in public health outreach, I can tell you that this kind of clarity saves lives. Every single person who reads this and decides to check their kit-whether they’re in a high-rise apartment in Manhattan or a rural home in Mississippi-is already making a difference.
Let’s normalize this: checking your first-aid kit isn’t a chore. It’s an act of love-for yourself, for your family, for your neighbors. Let’s make it a monthly ritual. Let’s teach our children to do it. Let’s build a culture where safety isn’t an afterthought-it’s a habit.
You’ve given us more than information. You’ve given us a mission. Thank you.
Susan Arlene
i just looked at my first aid kit and realized half the stuff is older than my last relationship. i’ve got ibuprofen from 2019, a bandage that says ‘sterile’ but looks like it survived a hurricane, and an epi pen that probably has more dust than adrenaline.
also i store everything in my bathroom because it’s convenient. and honestly? i’m not even mad. i’m just… kinda impressed i’m still alive.
maybe i’ll check it this year. maybe. if i remember.
Ashley S
THIS IS WHY AMERICA IS FALLING APART. People are terrified of a $10 bottle of painkillers but won’t vaccinate their kids. They’ll replace an EpiPen like it’s a phone case but drive 200 miles without a seatbelt. You’re not protecting yourself-you’re indulging in performative safety.
Stop buying into the fear machine. Your first-aid kit is not a shrine. It’s a tool. Use it. Don’t worship it.
Rachel Wermager
Interesting. So you’re equating rational, evidence-based medication stewardship with ‘performative safety’? That’s not just misinformed-it’s dangerously reductive. A seatbelt prevents trauma. An expired EpiPen causes it. One is passive prevention. The other is active, life-or-death pharmacology.
And no, I’m not ‘worshipping’ my first-aid kit. I’m acknowledging that biology doesn’t care about your ideology. A degraded epinephrine molecule doesn’t negotiate. It just fails. And when it does, you don’t get a second chance to say ‘oops’.