Learn which opioids are safe for kidney failure, how to adjust doses by GFR, and practical tips for monitoring side effects.
Opioids and Renal Failure: What You Need to Know
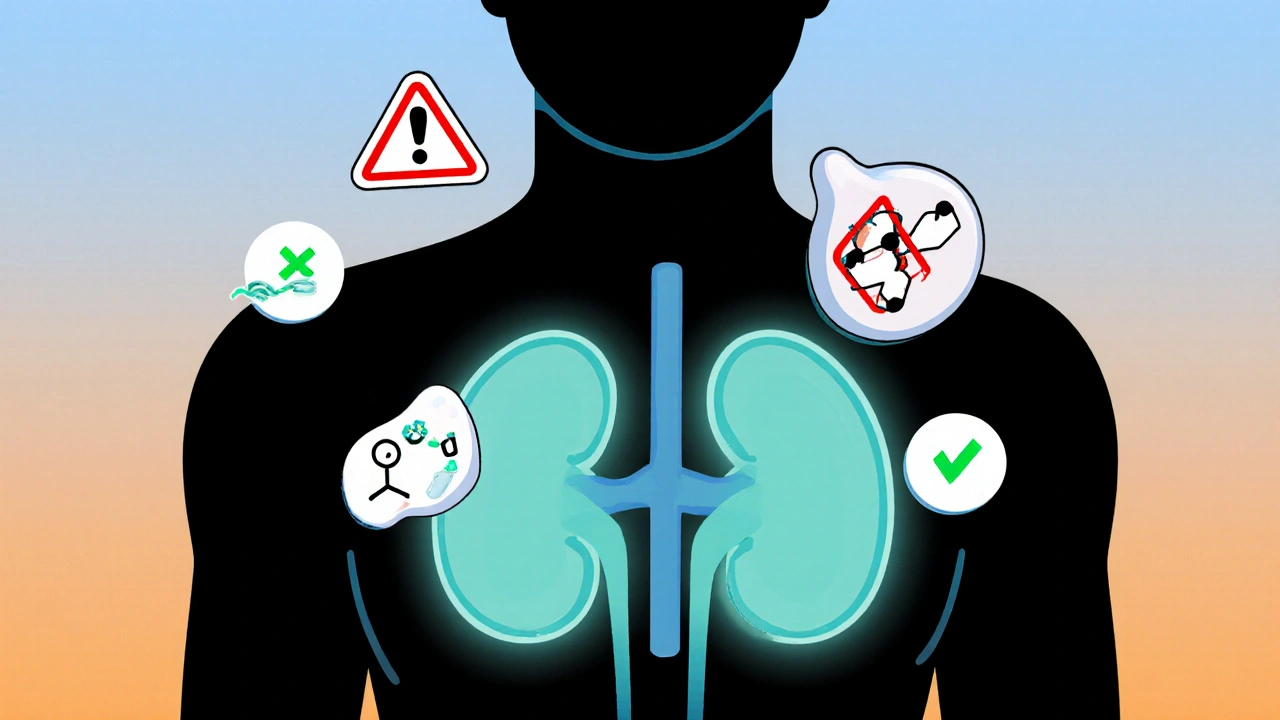
When you take opioids, a class of pain-relieving drugs that include morphine, oxycodone, and hydrocodone. Also known as narcotics, they work by binding to receptors in the brain and spinal cord to reduce pain signals. But for people with kidney disease, a condition where the kidneys can’t filter waste and fluids properly, these drugs don’t just stop working—they can make things worse. About 30% of chronic opioid users show signs of reduced kidney function over time, especially if they already have diabetes, high blood pressure, or are over 65.
Renal failure, when the kidneys lose their ability to maintain balance in the body isn’t always sudden. It often creeps in quietly, and opioids can speed it up. Some opioids, like codeine and morphine, break down into compounds that build up in the blood when kidneys are weak. This isn’t just about dosage—it’s about how your body handles the drug. For example, morphine metabolites can cause confusion or seizures in people with poor kidney function, even at normal doses. Meanwhile, drugs like fentanyl and methadone are often safer because they’re cleared by the liver instead. But that doesn’t mean they’re risk-free. Long-term use still affects blood pressure, fluid balance, and hormone levels—all of which stress the kidneys.
It’s not just about switching drugs. Managing pain with kidney disease means looking at the whole picture: Are you on diuretics? Are you dehydrated? Do you take NSAIDs on the side? These things stack up. Many patients don’t realize that even a single dose of ibuprofen with an opioid can drop kidney function fast. And if you’re on dialysis, your pain meds need to be timed around sessions—some drugs get removed during treatment, leaving you in pain again hours later.
What you’ll find in the posts below isn’t just theory. It’s real-world advice from people who’ve been there: how to spot early signs of kidney trouble while on opioids, which painkillers are safest when your kidneys are failing, how doctors adjust doses, and what non-drug options actually work. You’ll see comparisons between drugs like alfacalcidol and calcitriol—used in kidney patients for bone health—and how they interact with pain meds. You’ll find tips on medication timing, hydration, and monitoring lab values. No fluff. No marketing. Just what matters when your kidneys are under pressure.