Learn which opioids are safe for kidney failure, how to adjust doses by GFR, and practical tips for monitoring side effects.
Opioid Dosing in CKD: Safe Pain Management for Kidney Patients
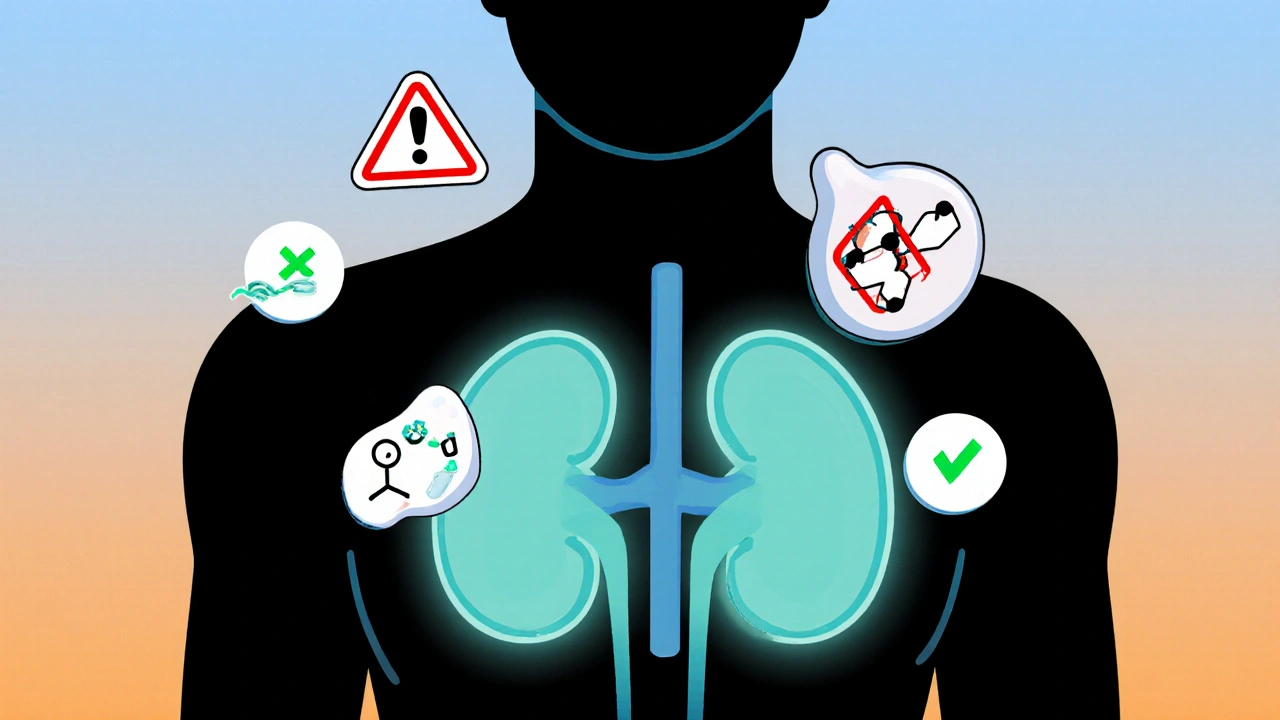
When someone has chronic kidney disease, a long-term condition where the kidneys slowly lose function. Also known as CKD, it changes how your body handles many drugs—especially opioids, which are commonly used for pain but can build up dangerously if not adjusted. Unlike healthy kidneys that filter out waste, damaged kidneys can’t clear these drugs the same way. That means even a normal dose might become toxic over time, leading to drowsiness, breathing problems, or even overdose.
This isn’t just a theoretical risk. Studies show that patients with CKD are up to three times more likely to have opioid-related complications. The problem? Many doctors still use standard dosing charts designed for people with normal kidney function. But not all opioids are created equal. Morphine, a common painkiller turns into active metabolites that stick around in CKD patients, making it risky. Hydromorphone, a stronger cousin of morphine, is also problematic. On the other hand, fentanyl, a synthetic opioid mostly leaves the body unchanged and is often safer. So is methadone, a long-acting opioid with complex metabolism—but it needs careful monitoring because it can build up slowly and affect heart rhythm.
It’s not just about picking the right drug. Dosing matters too. A patient with stage 4 CKD might need half the dose of someone with stage 2. And timing? Dosing every 12 hours instead of 8 can make a big difference. Some patients need even less—like starting at 25% of the usual dose and going up slowly. The goal isn’t to avoid pain relief. It’s to get relief without risking harm. That’s why doctors now use tools like the CKD-Opioid Dosing Algorithm and check kidney function regularly when prescribing.
And what if opioids aren’t the answer? There are other options. Acetaminophen, a common pain reliever is often preferred for mild to moderate pain in CKD, as long as it’s not overused. Non-drug approaches—like physical therapy, nerve blocks, or even mindfulness techniques—can reduce reliance on pills. But when pain is severe, opioids still have a role. Just not the old-school way.
What you’ll find in the posts below are real-world guides on how to navigate this. You’ll see comparisons of which opioids are safest in kidney disease, how to adjust doses step by step, what side effects to watch for, and what alternatives actually work. No fluff. No guesswork. Just clear, practical info from posts written for patients and providers who need to get this right.