Opioid Safety: How Naloxone Saves Lives, Recognizing Overdose Signs, and Safe Storage Tips

Every year, thousands of people in the U.S. die from opioid overdoses - not because they took too much, but because no one knew how to respond in time. The truth is, naloxone can bring someone back from the brink in minutes. But if you don’t know how to use it, where to keep it, or when to call 911, it won’t help. This isn’t just for people who use opioids. It’s for parents, friends, neighbors, and anyone who might be the first person on the scene when someone stops breathing.
What Naloxone Does - And What It Doesn’t
Naloxone is a medication that kicks opioids off the brain’s receptors. When someone overdoses on heroin, fentanyl, oxycodone, or even prescription painkillers, their breathing slows or stops. Naloxone doesn’t cure addiction. It doesn’t work on alcohol, benzodiazepines, or cocaine. But if opioids are in the system, naloxone can reverse the overdose within 3 to 5 minutes. Studies show it works in up to 95% of cases when given quickly.
It’s not magic. It’s science. Naloxone binds more tightly to opioid receptors than the drugs causing the overdose. It pushes them out, restores breathing, and buys time. That’s it. No euphoria. No high. No effect if no opioids are present. That’s why it’s so safe for anyone to use - even without medical training.
Recognizing an Opioid Overdose
Most people don’t know what an overdose looks like. It’s not always someone slumped over with a needle in their arm. Often, it’s subtle:
- Unresponsive to loud noises or shaking
- Slow, shallow, or stopped breathing
- Blue or gray lips and fingertips
- Pinpoint pupils
- Gurgling or snoring sounds (like they’re drowning)
If you see any of these signs, assume it’s an opioid overdose - even if you’re not sure. Don’t wait. Don’t check for a prescription bottle. Don’t worry about legal consequences. Time is everything. A 2022 study in Addiction found that survival rates drop from 95% to 65% if naloxone is given after 5 minutes.
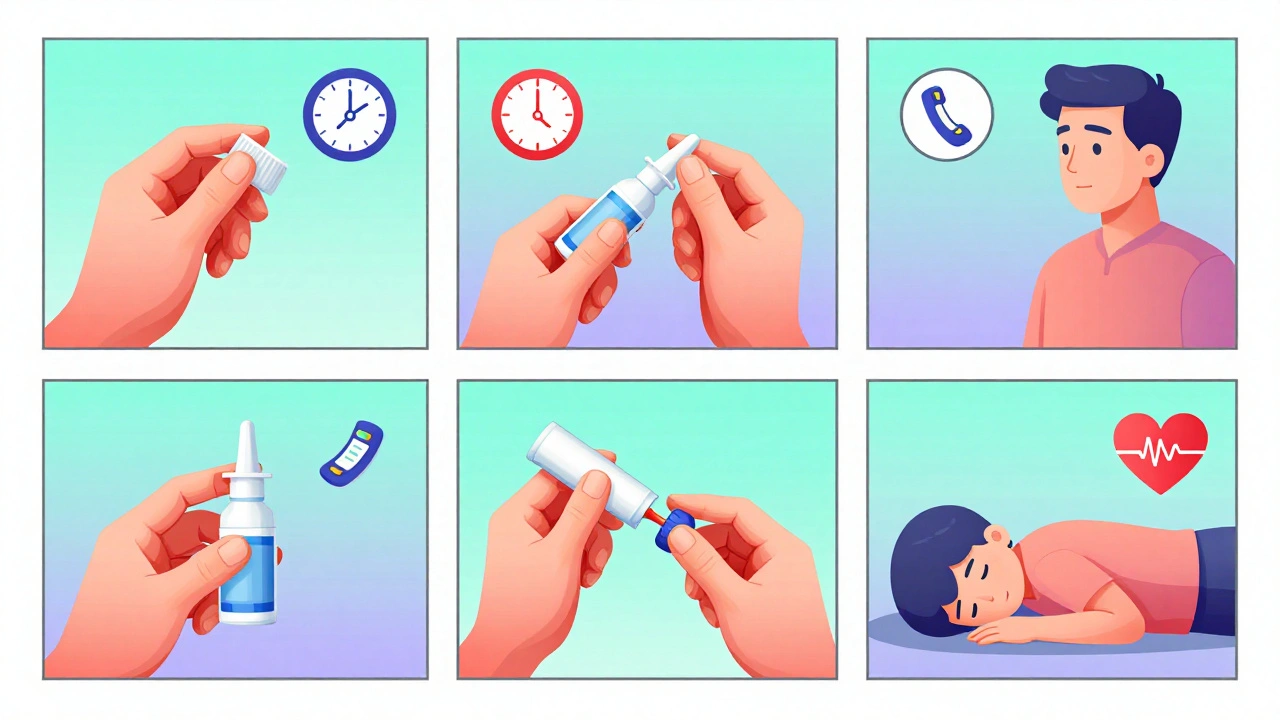
How to Use Naloxone - Step by Step
The most common form today is the nasal spray - no needles, no training needed. Here’s how:
- Call 911 immediately. Naloxone isn’t a substitute for emergency care.
- Place the person on their back. Tilt their head back slightly to open the airway.
- Remove the cap from the nasal spray. Hold it with your thumb on the bottom and two fingers on the top.
- Gently insert the nozzle into one nostril. Press the plunger firmly until you hear a click.
- Wait 2-3 minutes. If they don’t wake up or start breathing normally, give a second dose in the other nostril.
- Turn them onto their side (recovery position) to prevent choking if they vomit.
- Stay with them until paramedics arrive. Naloxone wears off in 30-90 minutes. Many opioids last longer - the overdose can come back.
Some people worry about giving too much. But giving extra doses is safe. If the person doesn’t respond, it’s likely because they took a powerful opioid like fentanyl. The CDC says 40% of fentanyl overdoses need more than one dose of naloxone.
Why Naloxone Isn’t Always Enough
Naloxone is powerful, but it’s not perfect. The biggest problem? Timing. Many people wait too long to act. Others don’t know what to do when the person wakes up - and then runs away.
When naloxone works, it triggers immediate opioid withdrawal. Symptoms include:
- Agitation or aggression
- Nausea and vomiting
- Sweating and shaking
- Intense pain from previously masked injuries
That’s scary - for the person and for the person helping them. Some people panic, run off, or refuse medical help. That’s why staying with them is critical. Withdrawal isn’t deadly, but it can lead to dangerous behavior.
Another issue: naloxone doesn’t last as long as fentanyl. A single dose might bring someone back, but if they took a high-potency synthetic opioid, they can slip back into overdose once the naloxone wears off. That’s why monitoring for at least 2 hours after the last dose is essential.
Safe Storage: Keep It Accessible, Not Hidden
Storing naloxone in a locked cabinet or a drawer you forget about defeats the whole purpose. It needs to be:
- Easy to find - not buried in a medicine cabinet
- At room temperature - avoid extreme heat or cold
- Out of reach of children - but not locked away
- Checked every 6 months - expiration dates matter
Many people keep naloxone in their car, purse, or bedside table. That’s fine. The goal is to have it where you are most likely to need it - not where you think you should keep it. The FDA-approved nasal sprays last 2-3 years. Check the expiration date on the box. If it’s expired, replace it. Expired naloxone won’t hurt you - but it might not work.
Some pharmacies offer free or low-cost naloxone with a prescription. Community programs in many cities give it away for free. If you’re worried about cost, call your local health department. In 2023, over 1.2 million kits were distributed through public programs.
What About Nalmefene?
You might hear about nalmefene - a newer drug with a longer duration of action. It’s being studied for opioid overdose, and early results show it can reverse fentanyl for up to 90 minutes - longer than naloxone’s 60-minute window. But as of late 2025, it’s not yet approved in the U.S. for this use. It’s still experimental. Stick with naloxone. It’s proven, available, and trusted by emergency responders nationwide.

Real Stories, Real Impact
On Reddit’s r/OpiatesRecovery, users have documented 87 successful reversals using naloxone. One person wrote: “I gave my brother the nasal spray after he stopped breathing. He opened his eyes 90 seconds later. I cried for an hour.” Another said: “I reversed three overdoses in a year. I almost didn’t buy the spray because it cost $140. Now I’m glad I did.”
Community programs report that 89% of naloxone administrations result in successful reversal. But 42% of users say they forget how to use it after a few months. That’s why training matters - even 15 minutes of practice makes a difference. Health departments offer free sessions. Watch a YouTube video. Practice on a dummy kit. You don’t need to be a nurse to save a life.
What Comes After Naloxone?
Naloxone saves lives - but it doesn’t fix the problem. People who survive an overdose are 100 times more likely to die from another one within a year. That’s why naloxone must be part of a bigger plan: access to treatment, counseling, housing, and recovery support.
The White House’s 2024 strategy aims to distribute 2 million naloxone kits annually. Research is underway for longer-acting versions. But right now, the most powerful tool you have is knowing what to do - and having the courage to do it.
What to Do If You’re Unsure
Still not sure? Call the Poison Help hotline: 1-800-222-1222. It’s free, confidential, and available 24/7. You can also visit the NIDA website for free training videos. You don’t need permission to carry naloxone. You don’t need a prescription in any state. And you won’t get in trouble for helping.
If you see someone who isn’t breathing - act. Call 911. Give naloxone. Stay with them. You might just be the reason they’re alive tomorrow.
Can naloxone be used on someone who didn’t take opioids?
No. Naloxone only works if opioids are present in the body. If someone overdosed on alcohol, benzodiazepines, or stimulants, naloxone won’t help. But if you’re unsure whether opioids were involved, it’s still safe to give it. It won’t harm someone who didn’t take opioids - and it could save their life.
How long does naloxone last, and can the overdose come back?
Naloxone lasts 30 to 90 minutes. Many opioids, especially fentanyl and its analogs, last much longer. That means the person can slip back into overdose after naloxone wears off. Always call 911 and stay with the person for at least 2 hours. Multiple doses may be needed.
Is naloxone safe for children and elderly people?
Yes. Naloxone is safe for all ages. It doesn’t affect people without opioids in their system. For children, use the same dose as adults - nasal spray is approved for all ages. For elderly individuals, especially those on long-term opioid pain medication, naloxone can trigger withdrawal symptoms, but that’s still safer than letting them stop breathing.
Can I carry naloxone in my car or purse?
Absolutely. Many people keep naloxone in their car, purse, or backpack. Store it at room temperature - avoid leaving it in direct sunlight or freezing conditions. Check the expiration date every 6 months. If it’s expired, replace it. Having it where you are most likely to need it increases the chance it’ll be used in time.
Where can I get naloxone for free?
Many pharmacies offer free naloxone with a prescription. Community health centers, needle exchange programs, and local health departments often give it away at no cost. In 2023, over 1.2 million kits were distributed through public programs across the U.S. Call your local health department or search for “naloxone free near me” - you’ll likely find help.
What if I’m afraid to call 911?
It’s normal to fear legal trouble. But in every state, Good Samaritan laws protect people who call for help during an overdose. The priority is saving a life. Emergency responders are trained to help, not punish. Naloxone is a tool - but 911 is the lifeline. Never hesitate to call.


Webster Bull
Naloxone ain't magic, but it's the closest thing we got. I keep two in my glovebox. One time, my cousin went blue in the parking lot after a party. I sprayed it, he gasped like a fish outta water, and 90 seconds later he was cursing me for waking him up. Worth it. 🙌
Jade Hovet
OMG YES!! I took the free class at my local pharmacy and now I carry it everywhere 😭 I even taught my 16yo nephew how to use it. He said he feels like a superhero now. 💪💉 #NaloxoneHero
Shelby Ume
While the technical guidance here is accurate, we must not reduce the opioid crisis to a pharmacological fix. Naloxone is a bandage on a hemorrhage. The real work lies in decriminalization, housing-first policies, and dismantling the profit-driven pharmaceutical infrastructure that flooded communities with opioids in the first place. We cannot treat symptoms while ignoring the disease.
Himmat Singh
It is my solemn duty to point out that the assertion regarding the 95% efficacy rate is statistically misleading. The sample populations in cited studies often exclude poly-substance users, non-English-speaking populations, and those in rural settings with delayed emergency response. To present this as universally applicable is an epistemological overreach.
Jamie Clark
You people are treating this like a goddamn first aid kit. Naloxone isn't a party favor. It's a symptom of a broken system where Big Pharma got rich while cities turned into graveyards. You hand out sprays like candy and pat yourselves on the back while the opioid pipeline keeps flowing. Where's the accountability? Where's the prosecution of the executives who lied about addiction rates? You want to save lives? Start by putting the architects of this disaster in prison.
Willie Onst
Just wanted to say thank you for writing this. My sister’s in recovery and she told me about how she lost three friends in a year. I got my kit last month - kept it in my purse like you said. Didn’t think I’d ever need it… until last weekend. We got to her in time. She’s alive. I’m not gonna lie - I cried for an hour. You’re right. It’s not about being a hero. It’s about being ready.
Jennifer Taylor
EVERYONE KNOWS THIS IS A GOVERNMENT TRAP. Naloxone? It's just to make people think they're safe so they keep using. Then they get addicted deeper. Then the feds can lock them up for 'non-compliance' with 'rehab.' I saw a video on TruthSocial - they inject trace chemicals into the spray to track users. They're building a database. They want to control the addicts. Don't be fooled. 🕵️♀️
nithin Kuntumadugu
Pathetic. You Americans treat death like a technical glitch. 'Just spray it and poof - problem solved.' Meanwhile, in India, we don't need fancy nasal sprays - we have community, we have family, we have responsibility. You turn a tragedy into a consumer product. 'Buy 2, get 1 free!' What a joke. 😒
Hamza Laassili
I'm from Texas, and I'll tell you what - if you're dumb enough to do opioids, you deserve to die. But if you're dumb enough to be around someone who OD'd, you better know how to use this thing. I don't care if you're a junkie - I ain't letting someone die on my watch. So yeah, I got 3 sprays in my truck. And I'm not sorry. 💪🇺🇸
Rawlson King
One must ask: is this not a form of enabling? By providing naloxone, we implicitly signal that overdose is an acceptable risk. The ethical burden lies not in the administration of the drug, but in the normalization of its necessity. A society that requires naloxone as a standard item in every purse has already lost its moral compass.
Constantine Vigderman
Just got back from a training session - they gave us practice dummies and everything! 🤩 I didn’t know you could just spray it up the nose! I thought you had to jab it or something. I’m gonna get one for my mom’s house. She’s always worried about me. Now she can sleep better. 💙 Also, if you’re scared to call 911 - just say ‘I think someone overdosed’ - they don’t ask for names. Promise. You got this!
Michael Gardner
Let’s be real - most people who carry naloxone never use it. And most who do use it, don’t know what to do after. People wake up, panic, run off, and then overdose again because they’re in withdrawal. The real problem isn’t access - it’s education. We need follow-up protocols, not just spray-and-pray.
John Fred
As a peer recovery specialist, I can confirm: the most effective intervention isn’t naloxone - it’s connection. The person who survives the overdose? They need someone to say, ‘I’m here.’ Not just a spray. Not just 911. A human. That’s why I carry my phone, my wallet with recovery cards, and two naloxone kits. The spray buys time. The conversation buys life. 💬❤️