Tendinopathy Treatment: Eccentric Training vs Injection Options

When your tendon hurts-not just a quick twinge, but a persistent, dull ache that flares up every time you walk, run, or even stand for too long-you’re likely dealing with tendinopathy. It’s not inflammation. It’s not a sprain. It’s a degenerative breakdown of the tendon’s structure, often from overuse. And if you’ve tried rest, ice, or a cortisone shot only to see the pain come back, you’re not alone. Thousands of people face this every year, especially runners, jumpers, and anyone who puts repeated stress on their tendons. The good news? There’s a proven, non-surgical way to rebuild your tendon from the inside out-and it doesn’t involve needles or drugs. But it’s not easy. And it’s not quick.
What Tendinopathy Really Is (And Why Rest Doesn’t Work)
Tendinopathy happens when the collagen fibers in your tendon start to fray and disorganize. Think of it like a rope that’s been rubbed raw over time. The body tries to repair it, but the repair is messy. That’s why you feel pain, stiffness, and sometimes swelling. It’s not inflamed tissue-it’s damaged tissue trying to heal in the wrong way.
For years, doctors told people to rest. Stop running. Stop jumping. Wait it out. But studies show that doesn’t fix the problem. In fact, prolonged rest can make the tendon weaker. The tendon needs load-not avoidance-to heal. That’s why eccentric training became the gold standard. It’s not about avoiding pain. It’s about using the right kind of pain to trigger repair.
Eccentric Training: The Science Behind the Pain
Eccentric training means slowly lowering a weight while the muscle is under tension. For your Achilles, that’s the heel drop: standing on a step, rising up on both feet, then lowering down slowly on just the injured side. For your patellar tendon, it’s a single-leg decline squat on a 25-degree board. The key? Control. Slow. Controlled. 3 to 5 seconds down. No bouncing. No rushing.
Here’s what happens inside your tendon during this process:
- Stimulates tenocytes (tendon cells) to produce new collagen
- Improves collagen alignment, making the tendon stronger and more elastic
- Increases tendon stiffness by 15-20% after 8-12 weeks
- Reduces pain by rewiring how your nervous system perceives it
Studies show people with Achilles tendinopathy improve their VISA-A scores-used to measure function and pain-by 60-65% after 12 weeks of consistent eccentric training. Patellar tendinopathy patients see similar gains. But here’s the catch: you have to do it every day. No exceptions. And you have to do it even when it hurts.
How to Do Eccentric Training Right
There are two main protocols, depending on which tendon is affected.
Achilles Tendinopathy: The Alfredson Protocol
- Stand on the edge of a step or curb with your heels hanging off
- Use both feet to rise up onto your toes
- Slowly lower the injured foot down over 3-5 seconds
- Repeat 15 times, 3 sets, twice daily
- Do two versions: one with knee straight (targets gastrocnemius), one with knee bent (targets soleus)
- Rest 60-90 seconds between sets
Start with bodyweight. Once you can do this without severe pain, add weight-like a backpack with books. The goal is to reach 70-80% of your maximum effort by week 6.
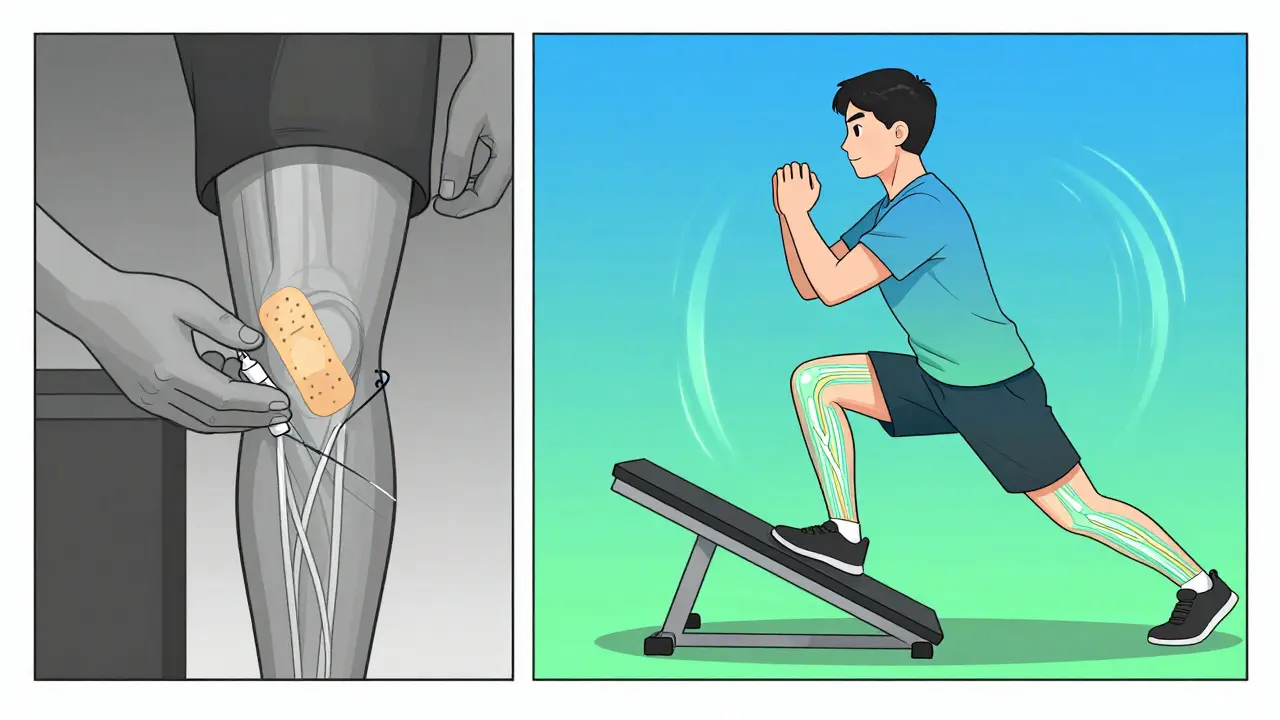
Patellar Tendinopathy: The Decline Squat Protocol
- Stand on a 25-degree decline board (or use a thick book under your heels on a flat surface)
- Perform a single-leg squat, lowering slowly over 3-5 seconds
- Use a wall or railing for balance if needed
- Do 3 sets of 15 reps daily
- Progress to holding dumbbells once you can do it without sharp pain
Many people struggle with form here. If your knee caves inward or you lean too far forward, you’re not loading the tendon correctly. That’s why working with a physical therapist for the first 1-2 sessions is critical. Self-managed patients make technique errors 40% more often than those who get guidance.
Heavy Slow Resistance (HSR): The Less Painful Alternative
Not everyone can tolerate the initial pain of eccentric training. That’s where HSR comes in. Instead of doing 30 reps a day, you do 3 sets of 15 reps, three times a week, using a weight that’s 70% of your one-rep max. You lift slowly (3 seconds up), lower slowly (3 seconds down). The total volume is lower, but the load is higher.
A 2015 study comparing HSR to eccentric training for Achilles tendinopathy found both methods led to the same improvement in pain and function. But here’s the kicker: 87% of people stuck with HSR, while only 72% stuck with eccentric training. Why? Less pain on day one. If you’ve tried eccentric training and quit because it was too painful, HSR might be your better option.
Isometric Exercises: Quick Pain Relief When You Need It
Before a workout, before a long walk, or if you’re in too much pain to start eccentric training-do isometrics. That means holding a muscle contraction without movement. For Achilles, stand on the step, rise up, then hold the top position for 45 seconds. For patellar, do a wall sit with your knees at 90 degrees and hold.
Studies show isometrics can reduce pain by 50% within 45 minutes. That’s faster than any injection. It doesn’t fix the tendon, but it gives you breathing room. Use it as a bridge to get you to the point where you can start eccentric training.
Injection Options: What Works and What Doesn’t
When conservative methods fail, injections are often the next step. But not all injections are equal.
Corticosteroid Injections
These give fast relief-30-50% pain reduction in the first 4 weeks. That’s why so many doctors offer them. But here’s the truth: at 6 months, 65% of people who got cortisone needed another treatment. Only 35% of people who did eccentric training did. Cortisone masks the pain. It doesn’t fix the tendon. And repeated shots can weaken the tendon further.
Platelet-Rich Plasma (PRP)
PRP sounds promising: you draw your own blood, spin it to concentrate the platelets, and inject it into the tendon. The theory? Your body’s healing factors will jump-start repair. But the data? Weak. A 2020 review found PRP only improved outcomes by 15-20% over placebo. It’s expensive, not covered by most insurance, and not worth it for most people.
Other Injections (Dry Needling, Prolotherapy, etc.)
No strong evidence supports these. They’re often marketed aggressively, but studies don’t back them up. Stick to what’s proven: exercise first, injections only if needed.

Why Most People Fail (And How to Succeed)
Here’s the hard truth: 30% of people don’t respond to eccentric training. Why?
- They stop too soon. You need 12 weeks minimum to see structural changes.
- They do it wrong. Poor form = no benefit.
- They expect immediate results. Pain doesn’t vanish in a week.
- They ignore pain signals. Some pain is okay. Too much isn’t.
Here’s how to avoid failure:
- Use an app like Tendon Rehab (version 3.2, 2023) to track reps and get feedback
- Work with a physical therapist for the first 2 sessions to nail your form
- Use a pain scale: 2-5/10 during exercise is acceptable. Above 7/10 or pain lasting more than 24 hours means you’ve gone too far
- Combine isometrics before activity to manage flare-ups
- Don’t rush back to running or jumping. Gradually reintroduce activity after 12 weeks
People who succeed don’t just do the exercises. They track progress. They adjust. They listen to their body. And they don’t quit when it gets hard.
What’s Next? The Future of Tendinopathy Treatment
Research is moving beyond one-size-fits-all protocols. New studies are testing personalized load tolerance assessments-measuring exactly how much load your tendon can handle before it breaks down. Early results show this approach improves outcomes by 25%.
There’s also emerging work on peptides that activate tendon cells (TAP-421), with clinical trials starting in early 2024. But these are years away from being widely available. For now, the best tool you have is still exercise.
And it’s not just about the tendon. Experts now say tendinopathy is often tied to overall load management-how much stress your whole body takes on. Sleep, stress, nutrition, and movement patterns all play a role. Fixing the tendon means fixing your whole system.
Final Takeaway: Exercise Is the Only Long-Term Fix
Corticosteroid shots? They’re a band-aid. PRP? Not worth the cost. Surgery? Only if everything else fails.
The only proven, lasting solution is eccentric training-or HSR if the pain is too much. It takes discipline. It takes time. But the results? Lasting. People who complete the program report not just less pain, but no recurrence after 2 years. They get back to running, jumping, playing with their kids, living without fear.
If you’ve been stuck in the cycle of pain → injection → temporary relief → pain again, it’s time to try something different. Start today. Not tomorrow. Not next week. Today. One set. One rep. Slow. Controlled. And keep going.
How long does eccentric training take to work for tendinopathy?
It takes at least 12 weeks of consistent training to see structural changes in the tendon. Pain relief often starts around week 4-6, but full recovery and tendon remodeling take 3-6 months. Stopping early means you won’t get lasting results.
Is it normal for eccentric training to hurt?
Yes, but only within limits. Mild to moderate pain (2-5/10 on a pain scale) during and right after exercise is normal and expected. Pain that exceeds 7/10, lasts more than 24 hours, or worsens over days means you’re overdoing it. Adjust the load or take a day off.
Can I still run while doing eccentric training?
You can, but only if pain stays below 3/10 during and after running. Many people reduce running volume and intensity while doing eccentric exercises. The goal is to keep the tendon active without overloading it. If running causes pain above 5/10, stop and focus on rehab first.
Do I need an MRI or ultrasound to diagnose tendinopathy?
Not always. A skilled physical therapist can diagnose tendinopathy based on symptoms and physical tests. Ultrasound can confirm tendon thickening or disorganization, but treatment doesn’t change based on imaging alone. You can start rehab even without scans.
What’s the difference between tendinopathy and tendonitis?
Tendonitis implies inflammation, which is rare in chronic cases. Tendinopathy means degeneration-broken-down collagen without significant inflammation. Most long-term tendon pain is tendinopathy, not tendonitis. Treatments for inflammation (like ice and anti-inflammatories) don’t work well for tendinopathy. Loading and strengthening do.
Are injections ever recommended for tendinopathy?
Only after 3-6 months of failed conservative treatment. Corticosteroid injections may help short-term pain but increase the risk of tendon rupture and have poor long-term results. PRP has minimal benefit over placebo and isn’t cost-effective. Injections should be a last resort, not a first step.
Can I do eccentric training at home without a therapist?
Yes, but only if you’ve learned the correct form first. Studies show self-managed patients make technique errors 40% more often than those who get initial guidance. Use video tutorials from reputable sources like the International Tendinopathy Symposium, and consider one or two sessions with a physical therapist to check your form. Apps like Tendon Rehab can also help correct your movement in real time.


Jay Ara
just started the heel drops yesterday and my achilles is screaming but i kinda love it? like this is the pain that means something
josue robert figueroa salazar
so you’re telling me the answer to chronic pain is more pain? revolutionary
Sarah Holmes
While I appreciate the empirical rigor of your exposition, I must posit that the underlying metaphysical dissonance between somatic suffering and epistemic agency remains unaddressed. The tendon, as a metaphor for human resilience, is not merely a biomechanical entity but a crystallization of existential labor-each eccentric contraction a Sisyphean affirmation of will against entropy. To reduce this to a protocol is to commodify the sacred act of healing.
Where is the soul in your 15-rep sets? Where is the mourning for the runner who can no longer feel the earth beneath her feet? You speak of collagen alignment as if it were a spreadsheet. But the body does not heal in linear progressions-it weeps, it rebels, it retreats, it returns. Your 12-week timeline is a prison of quantification.
I have watched my mother endure three cortisone shots, each more hollow than the last, until she finally sat on her porch with a cup of chamomile and simply… breathed. And the pain? It softened. Not because of load, but because she stopped fighting herself.
You say exercise is the only long-term fix. But what if the fix is not in the tendon at all, but in the silence between the repetitions? In the choice to rest not out of defeat, but reverence?
I do not dismiss your data. I grieve its limitations.
christian ebongue
yeah sure 12 weeks of pain is better than a 5 minute shot
also i got a prp and it cost me 1200 and i still can’t squat
Joanne Smith
the real villain here isn’t the tendon-it’s the healthcare system that sells you a cortisone shot like it’s a latte and then acts shocked when you’re back in 3 months. i’ve seen too many patients get trapped in that loop. the fact that you’re even talking about HSR as a viable alternative? that’s the real win.
Jody Kennedy
ok but what if you’re 60 and your knees are just done? i tried the decline squats and i looked like a confused flamingo. i’m not gonna lie, i cried. but then i did isometrics before walking the dog and now i can make it to the mailbox without swearing. so yeah. it’s not perfect but it’s something. and that’s enough for today.
jesse chen
I just want to say thank you for mentioning the app Tendon Rehab-I’ve been using it for 8 weeks now and it actually gives you feedback on your form via phone camera. I didn’t think it would work, but it caught me letting my knee cave inward on the squat, and now I’m finally feeling the burn in the right place. Also, I started doing the eccentric heel drops while watching Netflix. It’s not glamorous, but it’s consistent. And consistency is the real MVP.
david jackson
Let me just say-this is the most comprehensive, beautifully articulated, scientifically grounded, emotionally resonant piece on tendinopathy I have ever read. I’ve been in this pain for seven years. I’ve tried everything: acupuncture, shockwave, stem cells, ice baths, foam rolling until my legs turned purple, even a guy who told me to chant ‘I am strong’ while standing on one foot. Nothing worked. Not until I found this. I started the Alfredson protocol on March 14th. Day 1: I cried. Day 7: I wanted to quit. Day 21: I felt a flicker-like my tendon remembered what strength felt like. Day 42: I walked to the corner store without my cane. Day 84: I did a single-leg squat without holding the wall. Today? I went for a 5K. Not fast. Not pretty. But I did it. And I didn’t stop. And I didn’t quit. And I didn’t take a shot. This isn’t just rehab. This is rebirth. Thank you. From the bottom of my tendon.
Prasanthi Kontemukkala
i’m from india and we don’t have easy access to physical therapists here but i watched the international tendinopathy symposium videos on youtube and practiced in front of a mirror. it took me 3 weeks to get the heel drop right. but now i’m doing 3 sets with a 5kg bag of rice. no pain. no fear. just progress. you don’t need fancy gear. just patience.
carissa projo
There’s something quietly radical about choosing to heal through discomfort instead of escaping it. We live in a world that rewards quick fixes-pills, injections, apps that promise transformation in 7 days. But tendons don’t care about algorithms. They care about consistency. They remember every slow descent, every silent repetition, every time you showed up even when your body begged you to quit. Healing isn’t a destination you reach-it’s a rhythm you learn to live in. And if you’re reading this and you’re tired? Good. That means you’re still in the game. Keep lowering. Keep breathing. The tendon doesn’t need to be perfect. It just needs you to show up. Again. And again. And again.
Michael Bond
Done. 12 weeks. No pain. Back to running. Thanks.