GLP-1 Receptor Agonists: How They Help Lose Weight and Lower A1C
What Are GLP-1 Receptor Agonists?
GLP-1 receptor agonists are a class of injectable medications that mimic a natural hormone in your body called glucagon-like peptide-1. This hormone is released by your gut after you eat and helps control blood sugar and appetite. Originally developed for type 2 diabetes, these drugs have become famous for their powerful weight loss effects. They’re not magic pills - they work by changing how your body processes food, signals hunger, and stores fat.
Today, the most common ones include semaglutide (sold as Ozempic for diabetes and Wegovy for weight loss), liraglutide (Victoza and Saxenda), dulaglutide (Trulicity), and tirzepatide (Mounjaro and Zepbound). Semaglutide is currently the strongest, with studies showing it can drop A1C by nearly 2% and help people lose over 15% of their body weight. Tirzepatide, a newer dual-acting drug, is even more effective for weight loss - some users lose over 20% of their starting weight.
How Do They Lower Blood Sugar?
These drugs don’t just push insulin out - they work smart. When your blood sugar rises after a meal, GLP-1 agonists tell your pancreas to release insulin only if needed. This is called glucose-dependent insulin secretion. Unlike older diabetes drugs like sulfonylureas, they rarely cause dangerous low blood sugar.
They also quiet down your liver’s glucose production by 10-20%. That’s a big deal because in type 2 diabetes, the liver keeps pumping out sugar even when you don’t need it. At the same time, they block glucagon - a hormone that tells your body to release more sugar. This dual action on insulin and glucagon is why A1C levels often drop by 1.0% to 1.8% within months.
They also help your muscles take up more glucose - up to 25% more in some studies. That means less sugar stays in your bloodstream, and your cells get the energy they need. These effects add up fast. In the SUSTAIN 1 trial, people on semaglutide saw their A1C fall from 8.7% to 6.9% in just 30 weeks.
How Do They Make You Lose Weight?
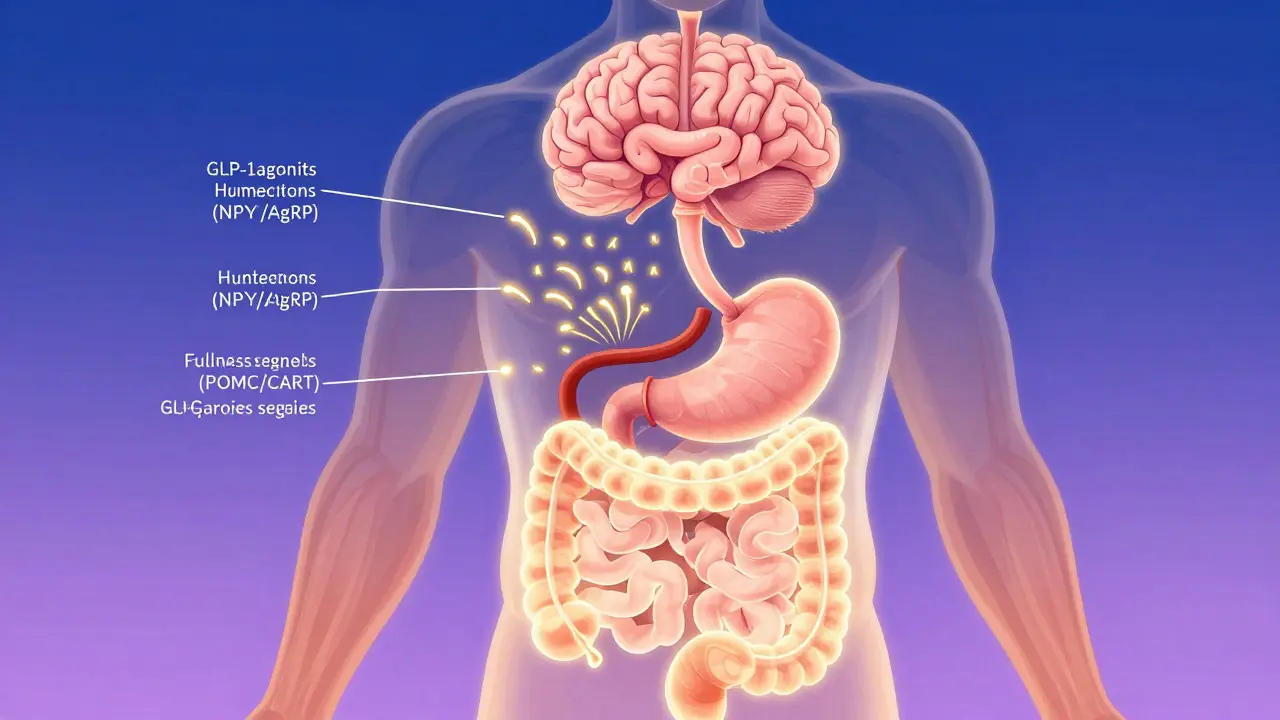
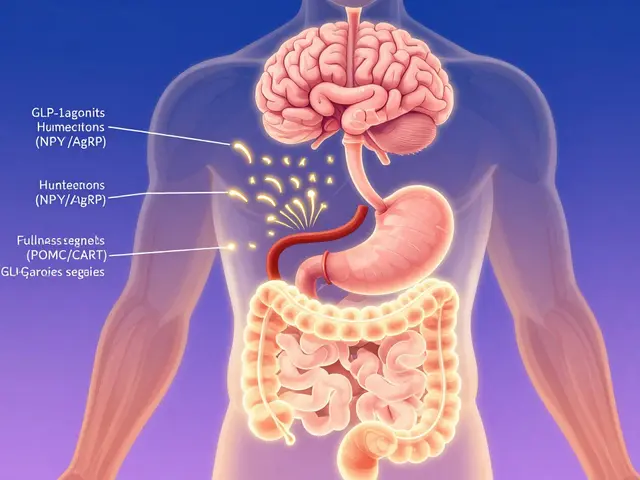
The weight loss isn’t accidental - it’s built into the mechanism. GLP-1 receptors are found not just in your pancreas, but also in your brain, especially in the hypothalamus, which controls hunger. When activated, these receptors turn down the volume on hunger signals.
They silence neurons that make you crave food (NPY and AgRP) and turn up the ones that tell you you’re full (POMC/CART). Clinical studies show this reduces appetite by 30-40%. You don’t feel deprived - you just stop thinking about food as much. One user on Reddit said, “I used to snack all day. Now, I eat lunch and forget about food until dinner.”
They also slow down your stomach. After eating, your stomach empties 15-30% slower. That means food stays in longer, you feel full longer, and blood sugar spikes don’t happen. This isn’t just about portion control - it rewires your relationship with food. Many users report losing cravings for sugary or fatty foods. It’s not willpower. It’s biology.
The numbers speak for themselves. In the STEP 8 trial, people taking semaglutide 2.4 mg lost an average of 15.8% of their body weight over 68 weeks. That’s about 35 pounds for someone weighing 220. Liraglutide, by comparison, led to 6.4% loss. Tirzepatide? Up to 20.9% in the SURMOUNT-2 trial. That’s comparable to gastric bypass surgery - without the operation.
How Do They Compare to Other Diabetes Drugs?
Most diabetes medications don’t help with weight - some make it worse. Sulfonylureas like glimepiride cause 2-4 kg of weight gain. Insulin? Often 4-10 kg. Even DPP-4 inhibitors like sitagliptin barely move the needle - maybe 0.5% A1C drop and ±0.5 kg weight change.
GLP-1 agonists beat them all. They’re more effective than SGLT2 inhibitors (like empagliflozin), which help with about 2-5 kg weight loss but don’t reduce appetite the same way. And unlike oral pills, these drugs deliver consistent, powerful results.
But they’re not the same across the board. Semaglutide outperforms liraglutide in both A1C and weight loss. In the SUSTAIN 10 trial, semaglutide lowered A1C by 1.8% versus 1.1% with liraglutide. In STEP 8, semaglutide users lost 15.8% of body weight - liraglutide users lost just 6.4%. The difference isn’t small. It’s life-changing.
Side Effects and How to Manage Them
Yes, they come with side effects - mostly in the first few weeks. Around 30-50% of users get nausea, 15-20% vomit, and 10-15% have diarrhea. These aren’t rare. They’re normal, especially when starting or increasing the dose.
The key is slow titration. Semaglutide (Wegovy) starts at 0.25 mg once a week. You stay there for four weeks. Then you go to 0.5 mg, then 1.0 mg, then 1.7 mg, and finally 2.4 mg. Rushing this process makes side effects worse. Most people feel better after 8-12 weeks.
Here’s what helps: take the shot at night. Eat smaller, lower-fat meals during the first few weeks. Avoid greasy food - it slows digestion even more and makes nausea worse. If nausea hits, try ginger tea or over-the-counter dimenhydrinate (Dramamine). Most people adapt. One user wrote: “The first month was rough. By month three, I forgot I was even taking it.”
Needle fear? Common. But most people master the injection after 2-3 tries. The pens are small, with thin needles. Novo Nordisk reports 85% of users self-administer successfully after training.
Cost, Insurance, and Access
These drugs are expensive. Without insurance, a month’s supply of Wegovy or Ozempic can cost $800-$1,200 in the U.S. That’s why so many people struggle to get them.
In the UK, NHS access is limited. They’re approved for type 2 diabetes, but weight loss use is mostly private. Some clinics offer them through private prescriptions, but waiting lists are long. Medicare in the U.S. covers about 62% of prescriptions, but often only after you’ve tried and failed other weight loss methods.
Insurance companies want proof you’ve tried diet, exercise, or older medications first. That’s frustrating - but it’s the reality. Some patients use patient assistance programs from manufacturers like Novo Nordisk or Eli Lilly to cut costs. Others travel to countries where generics are available - though this comes with risks.
What Happens When You Stop?
This is the biggest question people don’t ask until it’s too late. If you stop taking GLP-1 agonists, you will regain weight. Studies show people regain 50-70% of lost weight within a year of stopping.
It’s not because you “failed.” It’s because the drug was doing the work your body stopped doing. Your hunger signals return. Your stomach empties faster. Your brain forgets what full feels like. This isn’t weakness - it’s physiology.
That’s why experts say these drugs are for long-term use, like blood pressure or cholesterol meds. You don’t stop statins after your LDL drops - you keep taking them. The same logic applies here.

The Future: What’s Next?
Scientists are already working on better versions. Tirzepatide, which targets both GLP-1 and GIP receptors, is already showing even bigger weight loss numbers. Oral versions of semaglutide are now available - no injections needed. Early data shows they work, though not quite as well as the injectables.
Researchers are also testing them for fatty liver disease, heart failure, and even Alzheimer’s. A 2024 study in The Lancet found semaglutide cut liver fat by over half in people with NAFLD. The STEP-HFpEF trial showed improved heart function in obese patients with heart failure.
But supply is still a problem. In 2024, semaglutide was still on the FDA’s shortage list. Demand has outpaced production. Novo Nordisk is building new factories, but it’ll take years to catch up.
Who Should Consider Them?
If you have type 2 diabetes and are overweight - or if you have obesity (BMI ≥30) and want real, lasting weight loss - these drugs are among the most effective tools we have. They’re not for everyone. If you have a history of pancreatitis, thyroid cancer, or severe GI issues, talk to your doctor first.
They’re not a quick fix. They require commitment - to the dosing schedule, to managing side effects, to long-term use. But for those who stick with them, the results are dramatic: better blood sugar, less hunger, more energy, and a real shot at reversing diabetes.
For many, this isn’t just about looking different. It’s about living longer - and better.
Do GLP-1 agonists cure diabetes?
No, they don’t cure diabetes. But they can put it into remission for many people. When A1C drops below 6.5% without other medications, that’s considered remission. Many users maintain this for years - as long as they keep taking the drug and stay active. Stopping often brings blood sugar back up.
Can I take GLP-1 agonists if I don’t have diabetes?
Yes. Wegovy and Zepbound are FDA- and UK-approved for chronic weight management in adults with obesity (BMI ≥30) or overweight (BMI ≥27) with at least one weight-related condition like high blood pressure or sleep apnea. You don’t need diabetes to qualify.
How long does it take to see results?
You might notice less hunger within days. Weight loss usually starts in the first 2-4 weeks, but the full effect takes 16-20 weeks. A1C levels often drop within 8-12 weeks. Patience is key - the biggest changes happen after you’ve reached the full dose.
Are these drugs safe for long-term use?
Current data shows they’re safe for long-term use. The LEADER trial followed liraglutide users for over 5 years and found no increased cancer risk. In fact, they reduced heart attacks and strokes by 13% in high-risk patients. The biggest concern is weight regain after stopping - not the drug itself.
Can I drink alcohol while taking them?
Moderate alcohol is generally okay, but it can worsen nausea and increase the risk of low blood sugar if you have diabetes. Alcohol also adds empty calories, which can slow weight loss. Many users choose to cut back - not because they have to, but because they feel better without it.
Is there a generic version available?
No. All GLP-1 agonists are still under patent protection. Semaglutide and tirzepatide won’t have generics until at least 2030. Some people buy from overseas pharmacies, but this carries risks - counterfeit products, inconsistent dosing, and no regulatory oversight. Stick to licensed providers.
Final Thoughts
GLP-1 receptor agonists aren’t just another pill. They’re a shift in how we treat obesity and diabetes. They don’t just manage symptoms - they change how your body works. That’s why they’re the most talked-about drugs in medicine today.
They’re not perfect. They’re expensive. They require patience. But for the right person, they can be life-changing - not just in weight, but in energy, confidence, and long-term health.


Shawn Peck
These drugs are straight-up magic. I lost 40 lbs in 6 months on Wegovy. No gym, no keto, just stopped wanting donuts. My A1C dropped from 8.1 to 5.9. If you're still trying to 'eat less and move more' you're wasting your life.
Doctors won't tell you this but it's not about willpower anymore. It's biology. Your brain literally forgets to be hungry.
Sarah Blevins
While the clinical data supporting GLP-1 receptor agonists is statistically significant, the long-term safety profile remains incompletely characterized. The observed weight regain upon discontinuation suggests a pharmacological dependency rather than a metabolic reset. Furthermore, the cost-benefit analysis for public health systems remains contentious given the current pricing structure and limited generic availability.
Jason Xin
I used to roll my eyes at people on Ozempic. Then I watched my mom go from 220 to 165. She stopped needing insulin. Started hiking. Got her life back. I get why people hate it - it's expensive, it's weird, it's not 'natural'.
But if you've ever been too tired to play with your kids because your knees hurt or your blood sugar crashed at 3 p.m., you know this isn't about vanity. It's about being alive. I'm not mad at the drug. I'm mad we made it this hard to get.
Kathleen Riley
The ontological implications of pharmacologically induced satiety warrant profound philosophical consideration. One must interrogate whether the reduction of appetite constitutes an authentic alteration of human desire, or merely a technocratic suppression of biological imperative. In this paradigm, the self becomes a site of pharmaceutical governance - where the corporeal subject is reconfigured not through will, but through molecular intervention.
Is the individual who no longer craves sugar truly free? Or has agency been outsourced to Novo Nordisk?
Beth Cooper
Okay but have you heard about the CIA using these drugs to control people’s eating habits? I read a forum post from a guy in Canada who said his neighbor got prescribed Wegovy and then suddenly stopped eating meat and started voting Democrat. Coincidence? I think not.
Also, the FDA is hiding the fact that these drugs make you forget your own name. My cousin’s dog started whining after he took it. Maybe it’s a mind control thing. They’re probably trying to make us all skinny so we don’t need food stamps anymore.
Rohit Kumar
In India, we have a saying: 'The body is a temple, but the mind is the priest.' These drugs are like hiring a foreign priest who speaks only in molecules. We’ve spent centuries learning to eat with awareness - to slow down, to honor hunger, to feel full.
Now we outsource our will to a shot. Is this progress? Or just another way to avoid the hard work of living? I respect the science. But I wonder if we’re trading depth for convenience.
Carolyn Whitehead
I started semaglutide last year and honestly I didn’t think it would work for me but wow
my jeans fit and I don’t feel guilty eating pizza anymore because I just don’t want it like before
also my energy is insane like i’m walking around like a human now not a zombie
Beth Beltway
Let’s be real - this isn’t medicine. It’s a luxury product for rich people who can’t be bothered to eat vegetables. The fact that insurance requires you to fail at dieting first is just a way to make the poor suffer while the rich get their magic weight loss wand.
And don’t even get me started on the fact that people are buying Ozempic on Instagram from strangers. This isn’t healthcare. It’s a black market for people who think their worth is measured in pounds.
And now we’re talking about using it for Alzheimer’s? Next they’ll inject it into kids to make them stop eating candy. This is dystopia dressed in lab coats.