GLP-1 Agonists for Weight Loss: What You Need to Know About Benefits and Side Effects

When you hear about GLP-1 agonists, you might think of diabetes. But for millions of people struggling with weight, these drugs have become something else entirely: a game-changer. Medications like semaglutide (Wegovy) and tirzepatide (Zepbound) aren’t just helping people lose a few pounds-they’re delivering weight loss that rivals bariatric surgery for some. The average person on these drugs loses between 10% and 20% of their body weight. That’s not a fluke. It’s science. And it’s changing how we treat obesity.
How GLP-1 Agonists Actually Work
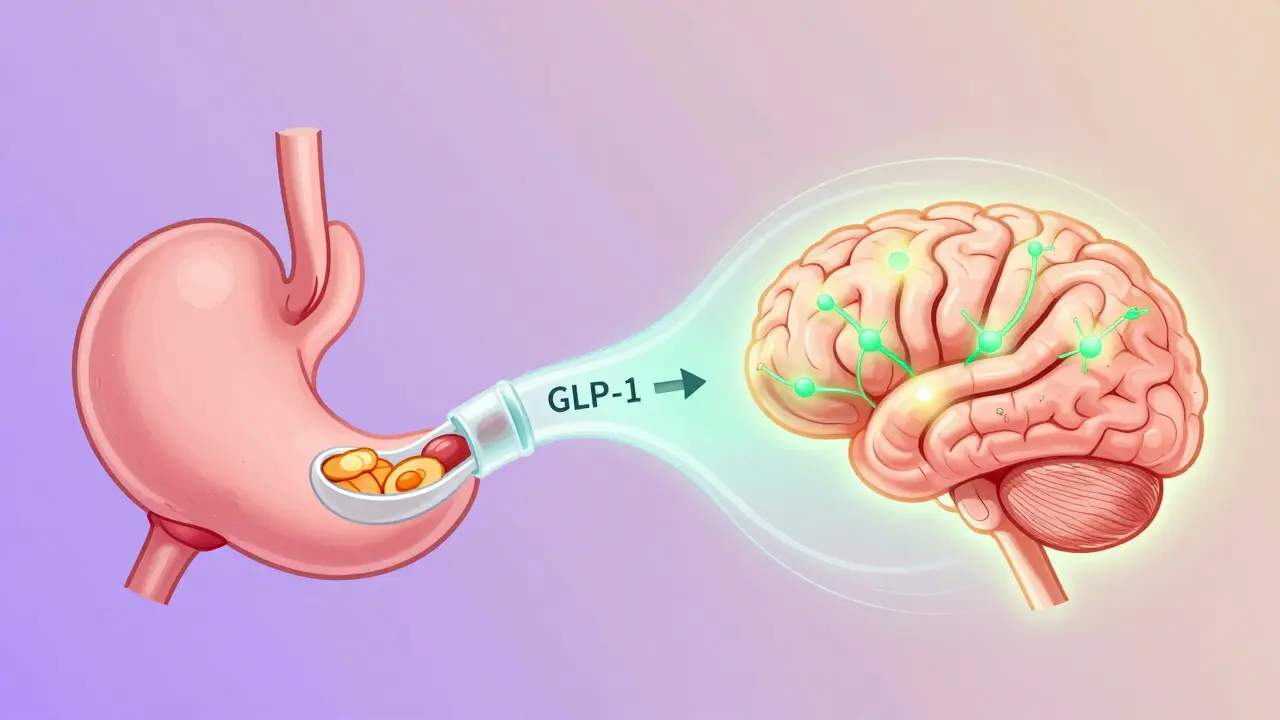
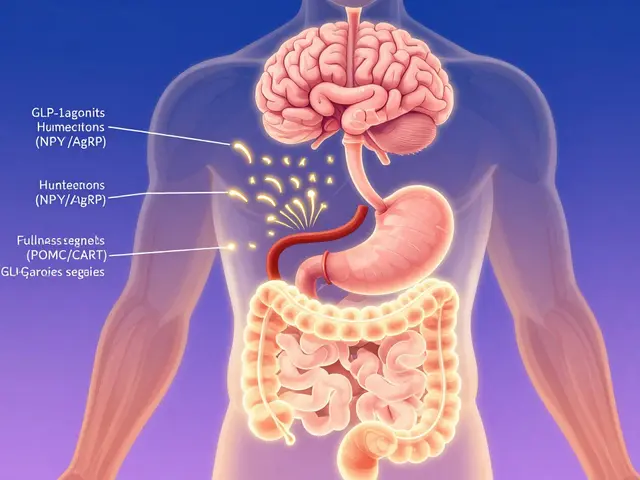
GLP-1 agonists mimic a natural hormone your body makes after you eat. This hormone, called glucagon-like peptide-1, tells your brain you’re full, slows down how fast your stomach empties, and helps your pancreas release just the right amount of insulin. Think of it like a built-in stop button for overeating.
Unlike diets that rely on willpower, these drugs work on your biology. They reduce hunger signals in the hypothalamus by activating POMC/CART neurons while quieting the ones that make you crave food-NPY and AgRP. They also stretch out your stomach’s emptying time by about 30 minutes after meals. That’s why people often say they feel satisfied with smaller portions. It’s not mental discipline. It’s chemistry.
These drugs also improve blood sugar control. That’s why they were first approved for type 2 diabetes. But the weight loss? That’s the side effect that turned into the main event.
Weight Loss Results You Can Expect
Not all GLP-1 agonists are the same. Here’s what real-world data shows:
- Semaglutide (Wegovy): 15.8% average weight loss over 68 weeks. In one trial, over half of users lost 15% or more of their body weight.
- Tirzepatide (Zepbound): 20.9% average weight loss at the highest dose. This one combines GLP-1 with another hormone (GIP), making it even more powerful.
- Liraglutide (Saxenda): Around 6.4% weight loss. Still effective, but clearly outperformed by newer options.
- Placebo groups: Lost about 2-3% on average.
Compare that to older weight-loss drugs. Orlistat (Xenical) blocks fat absorption but only delivers 5-10% loss-and often causes oily, embarrassing bowel movements. Phentermine-topiramate (Qsymia) gets you 7-10% loss but can cause brain fog and isn’t safe during pregnancy. GLP-1 agonists don’t just win on numbers. They win on tolerability and long-term health benefits.
The Real Cost: Money and Side Effects
There’s no sugarcoating this: these drugs aren’t cheap. In the U.S., Wegovy costs about $1,349 per month without insurance. Ozempic (the same drug, but approved for diabetes) runs around $936. That’s a huge barrier. Only 37% of private insurance plans cover Wegovy for weight loss as of 2023. Many patients pay out of pocket-or go without.
And then there are the side effects. About 70-80% of people experience nausea, especially in the first few weeks. Vomiting, diarrhea, and stomach pain are common too. One Reddit user wrote, “Weeks 3 to 8 were brutal. I almost quit.” But here’s the key: those symptoms usually fade after 8 to 12 weeks. Most people who stick with it say the discomfort becomes manageable.
Doctors recommend a slow titration. Wegovy starts at 0.25 mg once a week, then increases monthly until reaching 2.4 mg. Rushing the dose makes side effects worse. Patience matters.
Who Shouldn’t Take These Drugs?
Not everyone is a candidate. If you or a close family member has ever had medullary thyroid cancer or a rare genetic disorder called MEN2, you should avoid GLP-1 agonists entirely. These drugs caused thyroid tumors in rats during testing. While there’s no clear evidence this happens in humans, the FDA requires a black box warning.
Pregnancy is another concern. These drugs aren’t tested enough in pregnant women. If you’re planning to get pregnant, you’ll need to stop the medication at least two months before trying. Your doctor should check for pregnancy before starting.
People with a history of pancreatitis or severe gastroparesis should also proceed with caution. Slowing digestion too much can make those conditions worse.
What Happens When You Stop?
This is the part most people don’t talk about. Weight loss with GLP-1 agonists isn’t permanent if you stop taking them. In the STEP 4 trial, people who stopped the drug after a year regained about 60% of the weight they lost within the next year. That’s not failure. It’s biology.
Obesity is a chronic condition. Like high blood pressure or diabetes, it often needs ongoing treatment. Stopping the medication doesn’t mean you failed. It means your body went back to its old settings. That’s why experts say these drugs should be seen as long-term tools-not quick fixes.
Real People, Real Stories
On Reddit’s r/Ozempic community, over 20,000 users share their experiences. One person lost 78 pounds in 10 months. Another said they finally stopped snacking after dinner-not because they wanted to, but because they just didn’t feel hungry anymore.
On Drugs.com, 68% of users report losing at least 10% of their body weight. But 42% mention nausea, and 28% say cost was their biggest hurdle. One reviewer wrote: “I lost weight, but I had to sell my car to afford it.”
What’s consistent? The people who stick with it and manage their side effects are the ones who keep losing. The ones who quit early? They usually go back to where they started.
What’s Next?
The market is exploding. By 2030, GLP-1 drugs for weight loss could be a $100 billion industry. Novo Nordisk (maker of Wegovy) and Eli Lilly (maker of Zepbound) are racing to meet demand. Backorders for Wegovy stretched 18 months in late 2023. Supply hasn’t caught up with demand.
Oral versions are coming. Rybelsus, an oral form of semaglutide, is already approved for diabetes. Trials for its use in obesity are underway, with results expected in 2024. If it works, it could change everything-no more needles, lower cost, wider access.
Meanwhile, new drugs are in the pipeline. Pfizer’s danuglipron is an oral GLP-1 agonist in phase 2 trials. More options mean more competition-and eventually, lower prices.
What You Should Do
If you’re considering a GLP-1 agonist:
- See a doctor who understands obesity as a medical condition-not a moral failing.
- Ask about your insurance coverage. If it’s denied, ask for an appeal. Some plans cover it if you have diabetes, high blood pressure, or sleep apnea.
- Start low and go slow. Don’t rush the dose increase.
- Eat smaller meals. Avoid fatty or greasy foods during the first few weeks.
- Stay hydrated. Drink water throughout the day.
- Plan for long-term use. Think of this as managing a chronic disease, not a short-term diet.
These drugs aren’t magic. They don’t replace movement, sleep, or stress management. But they do give people a real shot at lasting change. For many, they’re the first tool that actually works.
Are GLP-1 agonists only for people with diabetes?
No. While they were first approved for type 2 diabetes, drugs like Wegovy and Zepbound are now specifically approved for chronic weight management in adults with obesity (BMI ≥30) or overweight (BMI ≥27) with at least one weight-related condition like high blood pressure or sleep apnea. The same drug, semaglutide, is sold as Ozempic for diabetes and Wegovy for weight loss-but the dose for weight loss is higher.
How long does it take to see weight loss results?
Most people start noticing reduced hunger and small weight loss within the first 4 to 8 weeks. But significant results-like losing 5% or more of body weight-usually take 12 to 16 weeks. The full effect often isn’t seen until after 6 months to a year of consistent use, especially since dosing increases gradually.
Can I take GLP-1 agonists if I have heart disease?
Yes-in fact, they’re often recommended for people with heart disease. Semaglutide was shown in the SUSTAIN-6 trial to reduce major cardiovascular events (like heart attack and stroke) by 26% in people with type 2 diabetes and existing heart disease. That’s why the American Diabetes Association now recommends GLP-1 agonists as first-line therapy for type 2 diabetes patients with cardiovascular risk.
Why do these drugs cause nausea?
GLP-1 agonists slow down how fast food leaves your stomach. This helps you feel full longer, but it can also cause food to sit in your stomach longer than usual, leading to bloating and nausea. The effect is strongest when you start the medication or increase the dose. Most people find their nausea improves after 8 to 12 weeks. Eating smaller meals, avoiding fatty foods, and staying upright after eating can help.
Is it safe to use GLP-1 agonists long-term?
Current data shows they’re safe for long-term use. Studies tracking patients for up to 3 years show sustained weight loss and no new safety concerns. The FDA’s black box warning about thyroid tumors in rats hasn’t translated to human cases, and no increased risk of thyroid cancer has been found in over 15,000 patients studied. Long-term use is now considered standard for obesity management, similar to how we treat high blood pressure with daily medication.


Kancharla Pavan
Let me be clear: this isn't medicine, it's corporate exploitation dressed up as science. These drugs are designed to keep people dependent for life, not cured. The pharmaceutical industry didn't invent obesity to sell drugs-they invented the narrative that obesity is a disease so they could sell drugs. And now we have people selling their cars just to afford a weekly injection. That's not progress, that's a Ponzi scheme with needles. If you're losing weight because your stomach feels like it's full of cement, you're not healthier-you're just medicated into submission. The real solution? Eat less, move more, stop treating food like emotional therapy. But hey, why fix the system when you can sell a $1,300-per-month Band-Aid?
Linda Franchock
Oh honey. You’re telling me people are selling cars to afford this? Sweetie. That’s not a miracle drug-that’s a luxury status symbol. I mean, if you’re going to spend $1,300 a month on a shot that makes you feel like a sick turtle, maybe you should’ve just started with...I don’t know...a salad? A walk? A therapist? But nooo, we gotta have the $1,000-per-week ‘I’m too lazy to change’ solution. And now the whole world’s obsessed with it. Next thing you know, people will be lining up for ‘weight loss IV drips’ at Sephora. I’m not saying it doesn’t work-I’m saying we’ve turned medical science into a TikTok trend. And it’s kinda sad.
Prateek Nalwaya
There's something deeply poetic about GLP-1 agonists, honestly. They don't just suppress appetite-they rewire the relationship between hunger and identity. You know how, for centuries, we blamed people for being 'weak-willed'? This drug doesn't ask you to be stronger. It just...quietly changes the rules of the game. It's like your body had a secret language you never learned, and now, suddenly, you're fluent. The nausea? That's just the old system screaming as it gets overwritten. And yeah, maybe it's expensive. Maybe it's not perfect. But for the first time, we're treating obesity not as a moral failure, but as a biological one. And that shift? That's revolutionary. I'm not saying everyone needs it. But for those who've been trapped in cycles of shame and starvation? This might be the first real door out.
Agnes Miller
i just wanted to say i started liraglutide last year and lost 22 lbs and honestly the nausea was bad at first but i just ate smaller meals and drank water and it got better. i’m on a low income and my insurance covered it because i have prediabetes so i’m lucky. i think people need to know it’s not magic but it helps if you pair it with real changes. also i didn’t know about the thyroid thing with family history-i’m gonna tell my mom. thanks for the info!!
Geoff Forbes
Wow. So we’ve officially moved from ‘eat less, move more’ to ‘take this expensive injection and call it a day.’ Classic America. We don’t fix problems-we monetize them. You want to lose weight? Go to the gym. Cook real food. Sleep. Stop blaming biology for your bad habits. These drugs are just another way for the rich to get rich while the rest of us pay for their ‘solution.’ And now they’re pushing oral versions? Next thing you know, Big Pharma will be selling weight-loss gummy bears. This isn’t medicine. It’s capitalism with a stethoscope.
Jonathan Ruth
Let’s cut the fluff. These drugs work. The data is undeniable. 20% weight loss? That’s not anecdotal-that’s clinical. The side effects? Temporary. The cost? A market failure, not a drug failure. People who say ‘just eat less’ have never had a body that fights back like mine did. I tried every diet. I ran marathons. I fasted. I counted calories. I failed. Then I got on Wegovy. I lost 40 pounds in a year. My knees don’t hurt anymore. I can walk up stairs without breathing like I just sprinted. This isn’t about laziness. This is about physiology. And if you’re too stubborn to admit that biology matters more than willpower, then you’re part of the problem.
Oliver Calvert
One thing everyone’s missing: the long-term safety data. We’ve had 3-year studies on semaglutide for weight loss. No increased cancer risk. No liver damage. No cognitive decline. The thyroid tumor thing? Rats. At doses 10x higher than humans take. We’ve had over 15,000 patient-years of exposure. That’s not a red flag-that’s a green light. The real issue isn’t the drug. It’s access. Insurance won’t cover it. Doctors don’t know how to prescribe it. People give up after 3 months because they’re scared of nausea. We need education. Not fear.
Brenda K. Wolfgram Moore
Thank you for writing this. I’ve been on tirzepatide for 8 months. Lost 51 lbs. My doctor didn’t take me seriously until I hit 300 lbs. Now I’m 249. I can hug my nieces without feeling like I’m going to collapse. I don’t hate my body anymore. I know this isn’t permanent. I know I’ll have to stay on it. But for the first time, I feel like I can be healthy. And if that means taking a shot every week for the rest of my life? I’ll do it. No shame. Just gratitude.
guy greenfeld
Think about it. What if this isn't about weight loss at all? What if Big Pharma knew that if they made a drug that made people feel full, they could rebrand obesity as a 'disease' and then lock people into lifelong dependency? And what if the FDA, the AMA, and even Reddit are all part of the same narrative? The 'side effects' are just distractions. The real goal? To normalize medical dependency. The 'weight loss' is the Trojan horse. The real product? A generation of people who believe their biology is broken and need corporate solutions to fix it. Wake up. This isn't science. It's a psychological operation. And you're being programmed.