Drug Nomenclature: Chemical, Generic, and Brand Names Explained

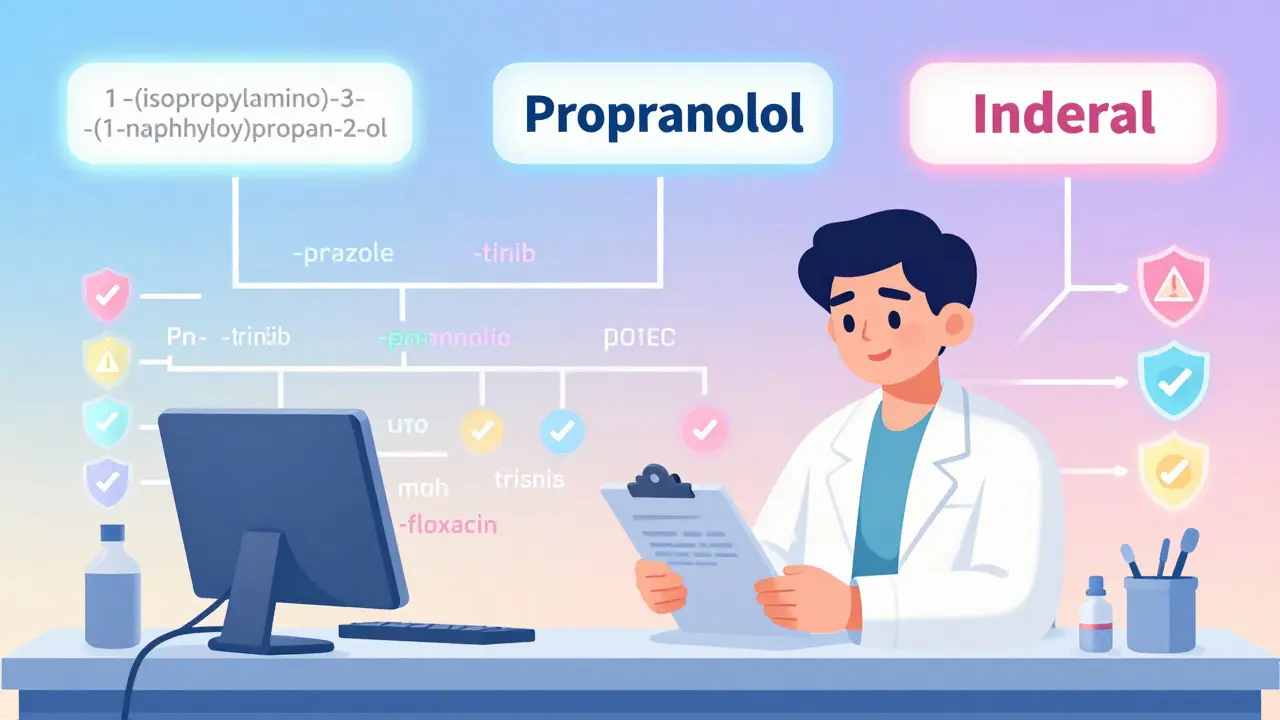
Ever picked up a prescription and wondered why the pill has three different names? You might see propranolol on the label, but your doctor called it by a brand name like Inderal. And if you dug into the fine print, you’d find a mouthful like 1-(isopropylamino)-3-(1-naphthyloxy)propan-2-ol. It’s confusing-and it’s supposed to be. Each name serves a different job, and getting them right can mean the difference between healing and harm.
Why Do Drugs Have So Many Names?
Drugs don’t get one name by accident. There’s a whole system behind it, built over decades to keep patients safe. The World Health Organization started this in 1950, and since then, over 10,000 standardized names have been assigned globally. The goal? Cut down on mistakes. The Institute of Medicine estimates that at least 1.5 million preventable medication errors happen every year in the U.S. alone. A lot of those happen because names look or sound too similar. That’s why naming isn’t left to marketing teams-it’s a science.
There are three layers to every drug’s identity: the chemical name, the generic name, and the brand name. Each one plays a different role. Think of it like a person: their full birth name (chemical), their everyday name (generic), and their nickname (brand).
Chemical Names: The Molecular Blueprint
The chemical name is the most precise. It’s built using rules from the International Union of Pure and Applied Chemistry (IUPAC). It tells you exactly how the molecule is put together-what atoms are where, how they’re bonded, the shape of the structure. For example, the chemical name for propranolol is 1-(isopropylamino)-3-(1-naphthyloxy)propan-2-ol. That’s 50+ characters long. No pharmacist is going to say that out loud. No patient will remember it. But scientists need it. When researchers are designing a new drug or studying how it breaks down in the body, they need this level of detail.
These names aren’t used in clinics or pharmacies. They’re for labs, patents, and regulatory filings. If you’re not a chemist, you’ll never need to use one. But knowing they exist helps explain why generic names are so much simpler. They’re a distilled version of the chemical structure-not the whole blueprint, but the key features.
Generic Names: The Safety Code
This is where things get smart. Generic names aren’t random. They follow patterns that tell you what the drug does. The ending-called a stem-gives away the drug class. The beginning-the prefix-makes it unique.
Take proton pump inhibitors. All of them end in -prazole: omeprazole, lansoprazole, pantoprazole. You see that ending, you know it’s for stomach acid. Tyrosine kinase inhibitors? They end in -tinib: imatinib, sunitinib. Janus kinase inhibitors? -citinib: tofacitinib. Even antibiotics follow this. Fluoroquinolones end in -floxacin: ciprofloxacin, levofloxacin.
These stems were designed by experts-pharmacologists, chemists, and safety specialists-to help doctors and pharmacists spot patterns at a glance. A 2020 study in the Journal of Clinical Pharmacology found that using stem-based naming reduces medication errors by 27%. That’s huge. Imagine a nurse rushing to give a patient their meds. If they see -prazole, they know it’s not a blood pressure drug. No mix-up.
But it’s not that simple. The USAN Council (which handles names in the U.S.) rejects about 30% of proposed generic names. Why? Because even small similarities can be dangerous. A name that sounds like hydroxyzine but ends in -zepam could be confused with alprazolam. One’s for allergies. The other’s for anxiety. Mix them up, and you’ve got a problem. The council runs every new name through AI tools that check against 15,000 existing drug names. It’s not just spelling-it’s sound, length, syllable stress.
Brand Names: The Marketing Mask
Now, the brand name. This is what you see on TV ads. Viagra, Prozac, Humira. These names are chosen by pharmaceutical companies to be catchy, memorable, and trademarkable. But they’re also tightly controlled. The FDA doesn’t just approve them-they reject about one in three submissions.
Why? Because brand names can’t sound too much like other drugs. If a new painkiller is called Zynox, but there’s already a blood thinner called Zynapin, the FDA will say no. Even small spelling differences-like Claritin vs. Clarinex-can cause confusion. In 2022, the FDA reported 347 medication errors linked to similar-looking brand names.
Brand names also can’t make promises. You won’t see a drug called InstantCure or GuaranteedPainRelief. That’s false advertising. The FDA requires that the generic name appear just as prominently as the brand name in all ads and packaging. So even if you remember Lexapro, you’ll also see escitalopram right next to it.
And here’s something people don’t realize: brand and generic drugs are chemically identical. The same active ingredient. Same dose. Same way it’s taken. The only differences? The color, shape, fillers, and flavor. Those are changed to avoid trademark infringement. So if you switch from Prilosec to omeprazole, you’re getting the exact same medicine. Just without the fancy packaging.
Company Codes: The Hidden ID
Before a drug even gets a generic name, it has a code. Pfizer uses PF followed by numbers-like PF-04965842-01. That’s the internal ID for abrocitinib, a drug for eczema. Other companies use different systems. Roche might use RO, Merck uses MK. These codes are used during clinical trials. They’re not meant for the public. But they’re how scientists track the drug from the lab to the pharmacy.
It takes years to get from a company code to a brand name. The process starts early-sometimes during preclinical testing. The generic name is picked during Phase I trials, around two to three years in. Brand names come later, usually six to twelve months before launch. The whole naming journey can take four to seven years. That’s longer than most PhD programs.
What’s Changing Now?
Drug naming isn’t stuck in the past. As new types of medicines come out, the rules are updating. RNA-based therapies? They now get the stem -siran. Peptide-drug conjugates? -dutide. Targeted protein degraders? The new stem is -tecan, and experts predict this class will grow 300% by 2030.
The USAN Council started using AI in 2021 to screen names. It checks pronunciation, spelling, and how names look next to each other on a prescription pad. In its first year, it cut potential confusion risks by 42%. That’s not just tech-it’s patient safety.
And it’s working. Since 2010, global medication errors linked to naming have dropped by 18.5%, according to the WHO. But challenges remain. Biologics-like antibodies-are harder to name because they’re made from living cells, not chemicals. Their names end in -mab (adalimumab, trastuzumab), but even then, differences can be subtle. A typo in one letter can change the whole meaning.
What Patients Should Know
Most patients don’t understand generic names. A 2022 FDA survey found that 68% of people find them confusing. They’re long. They sound weird. Atorvastatin? Levothyroxine? Hard to pronounce. But here’s the truth: your pharmacist knows them better than you do. They use the generic name because it’s the only one that’s consistent worldwide.
Don’t be afraid to ask: “Is this the same as the brand?” The answer is almost always yes. The only time it’s not is if you have an allergy to a filler-like lactose or dye-that’s in the brand version but not the generic. That’s rare.
And if you’re switching from brand to generic, don’t panic. The FDA requires generics to be bioequivalent. That means they work the same way in your body. The only difference? You’ll save money-often 80% less.
Why This Matters
Drug naming isn’t just about labels. It’s about saving lives. Every stem, every prefix, every rejected name is a shield against error. The system isn’t perfect. But it’s one of the most effective safety tools in modern medicine. And it’s built on collaboration-not between companies, but between scientists, regulators, and pharmacists across the world.
Next time you see a prescription, look at the name. If it ends in -prazole, you know what it does. If it’s a brand name, you know it’s just the marketing side. And if you see a long chemical name? That’s the science underneath it all.

Rob Deneke
I used to freak out when I saw generic names on my prescriptions until I learned the stems. Now I can tell what a drug does just by the ending. -prazole = acid reducer, -tinib = cancer stuff, -floxacin = antibiotics. Life changed. No more guessing.
Riya Katyal
So let me get this straight... we have a whole system designed to prevent doctors from killing people... but the names still sound like someone sneezed on a chemistry textbook? 🤦♀️
evelyn wellding
OMG this is SO cool 😍 I just learned that -mab means it's a biologic antibody thingy?? Like, I can actually read my own prescriptions now! My pharmacist thinks I'm a genius 🙌
Chelsea Harton
Names are just illusions. The pill doesn't care what you call it. But humans need labels to feel safe. Or control. Or both. Maybe it's all just language trying to tame chaos.
Corey Chrisinger
It's wild how much thought goes into this. The stems, the AI checks, the FDA rejecting names... it's like naming a child but with higher stakes. 🤔 One letter off and someone could die. We're basically playing linguistic Jenga with lives.
Bianca Leonhardt
People still don't get that generics are identical? Wow. Just wow. You're paying extra for a different color and a logo. And you think you're saving money? Please.
Travis Craw
I never realized how much work goes into naming drugs. I always just thought companies made up fun names like 'Viagra' and called it a day. Turns out it's way more serious than I thought. Good to know they're being careful.
Christina Bilotti
Oh wow. You mean the FDA actually stops companies from naming drugs 'InstantCure'? How quaint. In my day, we just called everything 'MiracleCide 9000' and hoped for the best. At least now we have a system. I suppose that's progress... if you're into bureaucracy.
brooke wright
I just looked up my dad's meds and realized he's been on three different drugs with the same stem -prazole. He didn't even know they were all for the same thing. He thought one was 'the strong one' and one was 'the mild one'. Poor guy. I'm printing this article out for him.
vivek kumar
The stem system is brilliant. But why are biologics so hard to name? If they're made from living cells, shouldn't their names reflect that? Maybe -cel or -live? Just a thought. Also, why does 'adalimumab' sound like a spell from Harry Potter?
Nick Cole
This is why I trust pharmacists more than doctors sometimes. They know the names inside out. I switched from brand to generic last year and saved $400. No side effects. No difference. Just cheaper. If you're scared of generics, you're scared of the wrong thing.