Why Patient Education Is Critical for Successful Ranolazine Therapy

Ranolazine Side Effect Guidance Tool
Common Side Effects
Imagine being prescribed a drug that can ease chest pain, but you stop taking it because you didn’t understand why the dose changes or what a harmless side effect looks like. That’s a common story with Ranolazine, the anti‑anginal medication that helps people with chronic chest pain live more comfortably. The missing link? Clear, practical patient education. Below you’ll find everything you need to turn a prescription into real relief.
Quick Takeaways
- Ranolazine works by improving heart cell metabolism, not by changing blood pressure.
- Patients who receive structured education are 30% more likely to stay on therapy.
- Key topics to cover: dosing schedule, common side effects, drug‑drug interactions, and self‑monitoring.
- Use visual tools (pill cards, mobile reminders) to boost adherence.
- Integrate education into every visit - before the first dose, at the 2‑week check, and during routine follow‑ups.
What Is Ranolazine?
Ranolazine is a p‑type anti‑anginal medication that enhances myocardial efficiency by shifting cardiac metabolism from fatty‑acid oxidation to glucose oxidation. Approved by the U.S. Food and Drug Administration in 2006, it’s indicated for patients with chronic stable angina who remain symptomatic despite beta‑blockers, calcium‑channel blockers, or nitrate therapy.
Why Patient Education Matters
Patient education refers to the systematic process of providing information, skills, and motivation so patients can manage their own health conditions effectively. In the case of Ranolazine, education tackles three big hurdles: understanding the drug’s unique action, recognizing manageable side effects, and staying consistent with dosing.
Core Components of Effective Ranolazine Education
- Explain the mechanism in plain language. Tell patients that Ranolazine helps the heart use energy more efficiently, like swapping a diesel engine for a hybrid that runs smoother.
- Lay out the dosing schedule. Starting dose is usually 500 mg twice daily; after two weeks it may increase to 1000 mg twice daily if tolerated. Emphasize taking the drug with food to lessen gastrointestinal upset.
- Identify the most common side effects. Dizziness, headache, constipation, and nausea are typical. Explain that these often fade after the first few weeks.
- Highlight red‑flag symptoms. New or worsening chest pain, severe palpitations, or unexplained shortness of breath should prompt a call to the healthcare provider.
- Discuss drug‑drug interactions. Ranolazine is metabolized by CYP3A4; avoid strong inhibitors like ketoconazole or clarithromycin unless absolutely necessary.
- Provide self‑monitoring tools. A simple log sheet for dose timing, side effects, and any chest pain episodes helps both patient and provider track progress.

Addressing Common Misconceptions
Many patients think “if I feel fine, I can stop the pill.” The reality is that Ranolazine works continuously to keep the heart’s metabolism balanced; stopping abruptly can bring back angina faster than before. Another myth is that higher doses always mean better relief. In fact, exceeding the prescribed dose increases the risk of QT‑interval prolongation, a heart rhythm issue that can be serious.
Managing Side Effects Through Education
When patients know what to expect, they’re less likely to abandon therapy. For example, if a patient experiences constipation, advise increasing fluid intake, adding dietary fiber, and, if needed, a mild over‑the‑counter stool softener. For dizziness, suggest rising slowly from sitting or lying positions and avoiding sudden head turns.
Integrating Education Into Clinical Workflow
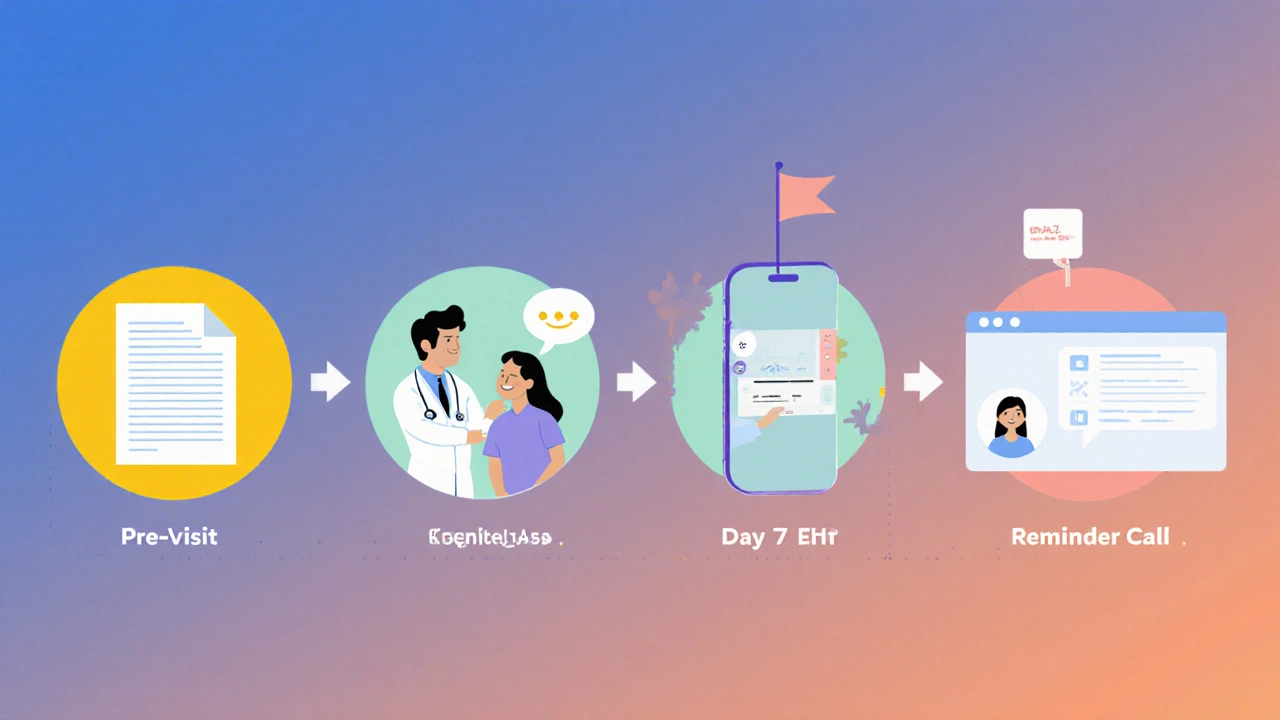
- Pre‑visit handout. Send a printable PDF or secure email a week before the first appointment. Include a pill‑card visual that marks “take with food.”
- In‑clinic teach‑back. After explaining dosing, ask the patient to repeat the schedule in their own words. This confirms understanding and highlights gaps.
- Follow‑up call. A brief phone check at Day 7 and Day 14 can catch early side effects and reinforce key messages.
- Electronic health record (EHR) prompts. Set a reminder for the provider to review education at each visit for patients on Ranolazine.
How Ranolazine Stacks Up Against Other Anti‑Anginal Drugs
| Feature | Ranolazine | Beta‑Blocker | Calcium‑Channel Blocker | Nitrate Therapy |
|---|---|---|---|---|
| Primary Action | Metabolic modulation | Heart‑rate reduction | Vasodilation | Vasodilation (venous) |
| Effect on Blood Pressure | Minimal | Lowers BP | Lowers BP | Variable |
| Typical Starting Dose | 500 mg BID | 5‑10 mg BID (varies) | 5‑10 mg BID (e.g., amlodipine) | 0.3‑0.6 mg sublingual PRN |
| Common Side Effects | Dizziness, nausea, constipation | Bradycardia, fatigue | Peripheral edema, flushing | Headache, hypotension |
| Drug‑Drug Interactions | CYP3A4 inhibitors/inducers | Limited | Limited | Limited |
| QT‑Interval Risk | Yes (monitor) | No | No | No |
The table shows why Ranolazine is a valuable add‑on when patients can’t achieve relief with traditional agents. Its metabolic effect means it doesn’t lower heart rate or blood pressure, making it compatible with many existing regimens - provided the patient knows how to avoid problematic interactions.
Checklist for Healthcare Providers
- Confirm diagnosis of chronic stable angina and prior use of beta‑blockers, calcium‑channel blockers, or nitrates.
- Review current medication list for CYP3A4 inhibitors (e.g., clarithromycin, itraconazole).
- Provide written dosing schedule with visual pill card.
- Discuss expected side effects and when to call.
- Schedule first follow‑up call within 7 days of initiation.
- Document patient‑teach‑back in the EHR.
- Order baseline ECG; repeat if dose escalated above 1000 mg BID.
Frequently Asked Questions
Can Ranolazine be taken with my cholesterol medication?
Most statins don’t interfere with Ranolazine because they’re not strong CYP3A4 blockers. However, avoid combining it with grapefruit juice, which can raise Ranolazine levels.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one and resume the normal schedule - never double‑dose.
Is it safe to use Ranolazine while pregnant?
The drug is classified as pregnancy Category C; it should only be used if the potential benefit justifies the risk. Discuss options with your cardiologist.
How long does it take to feel better?
Patients often notice reduced chest pain within 1‑2 weeks, but maximum benefit may require 4‑6 weeks of consistent dosing.
Can I stop Ranolazine once my symptoms improve?
Stopping abruptly can cause a return of angina. Any dose change should be discussed with your provider, who may taper the medication gradually.
Bottom line: Ranolazine can be a game‑changer for chronic angina, but only if patients understand how to take it, what to watch for, and why staying on therapy matters. By weaving clear education into every step of care, providers boost adherence, cut unnecessary ER visits, and help patients enjoy more pain‑free days.


Kimberly Lloyd
Think of medication adherence as a partnership between you and your heart; when you understand the why, the how becomes second nature.
Explaining that Ranolazine shifts the heart's fuel source can empower patients to see the drug as a supportive teammate rather than a mystery pill.
Using simple analogies-like swapping a diesel engine for a hybrid-helps demystify the metabolic action.
Encouraging patients to ask “what should I watch for?” builds confidence and reduces fear of side effects.
Remember, a patient who feels heard is far more likely to stay on therapy.
Lolita Gaela
From a pharmacokinetic standpoint, Ranolazine exhibits substrate specificity for the cardiac isoform of the late sodium current, necessitating vigilant monitoring of QTc intervals.
The drug's biotransformation via CYP3A4 mandates avoidance of potent inhibitors such as ketoconazole, clarithromycin, and certain HIV protease inhibitors.
Loading dose stratification (500 mg BID → 1000 mg BID) should align with trough plasma concentrations to mitigate arrhythmogenic risk.
Drug‑drug interaction matrices integrated into the EHR can preempt inadvertent co‑prescriptions that elevate serum levels.
Implementing a standardized order set with embedded decision support optimizes safety and adherence.
Giusto Madison
Don't just hand the pill and walk away-lay down the dosing schedule in plain language, and make sure they repeat it back.
Tell them the side effects like dizziness or constipation are usually transient, not a reason to ditch the med.
If they balk about the cost, point them to patient‑assistance programs now, not later.
Stick to the script and hold them accountable; anything less is sloppy care.
Xavier Lusky
There's a silent push to keep patients in the dark about Ranolazine's true mechanism because the pharma giants benefit from confusion.
They sprinkle vague side‑effect warnings in the fine print to scare you off, preserving market share for older drugs.
Only by demanding crystal‑clear education can we cut through the corporate smokescreen and let patients make informed choices.
Don't trust a label that doesn't spell out the metabolic shift-it’s a deliberate omission.
Ivan Laney
In the grand tapestry of American cardiovascular therapy, Ranolazine stands as a testament to our nation's ingenuity, yet its potential remains underexploited due to systemic educational gaps.
When clinicians fail to articulate the metabolic modulation pathway, patients revert to familiar beta‑blockers, unaware that a complementary mechanism exists to alleviate refractory angina.
The United States healthcare infrastructure, with its emphasis on rapid turnover, often sidelines thorough teach‑back sessions, inadvertently fostering non‑adherence.
Instituting a regimented, multi‑modal educational protocol-combining printed pill cards, digital reminders, and in‑person reinforcement-could dramatically elevate compliance rates, bolstering outcomes on a national scale.
Moreover, aligning insurance formularies to cover these educational tools would mitigate socioeconomic barriers that currently disenfranchise a substantial patient cohort.
By championing a policy that mandates comprehensive counseling at each prescription juncture, we not only honor the scientific rigor behind Ranolazine but also uphold our collective responsibility to the American patient populace.
Ultimately, the success of this therapy hinges on our willingness to invest time and resources into patient empowerment, a venture that promises a healthier, more productive nation.
Chirag Muthoo
It is imperative to convey the dosing escalation protocol with unequivocal clarity, emphasizing the two‑week titration window before any dosage increase is contemplated.
Patients should be apprised that concomitant administration of strong CYP3A4 inhibitors may necessitate dose adjustment to avert supratherapeutic exposure.
Documenting the teach‑back outcome in the electronic health record ensures accountability and facilitates continuity of care.
Such meticulous communication aligns with best practice standards and fosters sustained therapeutic adherence.
Angela Koulouris
Picture the medication schedule as a rhythmic melody; each dose is a beat that keeps the heart's symphony in harmony.
When patients visualize their regimen, they are less likely to miss a note and more likely to stay in tune.
Encouraging them to set a daily reminder transforms abstract advice into a concrete habit.
Harry Bhullar
First, understand that Ranolazine does not act like a traditional anti‑anginal by lowering blood pressure; instead, it optimizes myocardial energy utilization, which can be a game‑changer for patients who remain symptomatic despite other therapies.
Second, the initial dosing of 500 mg twice daily should be taken with food to reduce gastrointestinal upset, a simple tip that often goes unmentioned in brief prescriptions.
Third, after two weeks, assess tolerance before escalating to 1000 mg twice daily; this stepwise approach minimizes the incidence of dizziness and constipation.
Fourth, educate patients on the importance of reporting any new palpitations or chest pain promptly, as these may signal QT interval prolongation, a serious but manageable risk.
Fifth, provide a written pill card that clearly marks “take with meals” and includes a space for patients to log side effects, fostering active participation.
Sixth, emphasize that occasional mild nausea is expected and usually resolves within the first month, reducing the temptation to discontinue prematurely.
Seventh, integrate a medication reminder app that alerts patients at the designated dosing times, reinforcing consistency without relying on memory alone.
Eighth, review the patient's concurrent medication list for CYP3A4 inhibitors such as clarithromycin or certain antifungals, and advise temporary discontinuation or dose modification if necessary.
Ninth, schedule a follow‑up phone call at day 7 and day 14 to triage any emerging adverse effects and adjust the plan if tolerability issues arise.
Tenth, obtain a baseline ECG before initiating therapy and repeat it if the dose exceeds 1000 mg BID, ensuring any QT changes are detected early.
Eleventh, discuss lifestyle measures-regular low‑impact exercise, sodium moderation, and stress reduction-that synergize with Ranolazine to improve overall anginal control.
Twelfth, clarify that abrupt cessation can precipitate a rebound of chest pain, so any dose changes should be tapered under clinician supervision.
Thirteenth, involve family members or caregivers in the education session; their support can be pivotal in maintaining adherence during the initial adjustment period.
Fourteenth, document the teach‑back results in the electronic health record, noting any misconceptions corrected, to provide a clear audit trail.
Fifteenth, encourage patients to keep a symptom diary, recording episodes of chest discomfort, which can be reviewed at each visit to gauge therapeutic efficacy.
Finally, remind patients that consistency is key; the benefits of Ranolazine accumulate over weeks, and steadfast adherence often translates into more pain‑free days and a better quality of life.
Dana Yonce
Got the new pill schedule and feeling good 😊
erica fenty
Excellent-clear dosing, minimal side effects, real benefit.
Patients who follow the teach‑back protocol show higher adherence rates, indeed.
Sakib Shaikh
Yo, listen up-Ranolazine is like a secret weapon, the heart's own turbo‑charger!!
If you skip the schooling, you’re basically flying blind, bro.
Never ignore those mild nausea vibes; they’re just the body adjusting, not a red flag.
And don’t you dare mix it with strong CYP3A4 blockers unless you wanna get a wild QT ride!!!
Stick to the plan, log every dose, and you’ll dominate that angina once and for all.
Ashok Kumar
Sure, because nothing says "I care" like a quick glance at the prescription bottle and hoping the patient reads the fine print.
But actually, a gentle reminder that side effects are usually temporary can make a world of difference.
So, let’s be real and give them the tools they need, not just a name and a dosage.
Jasmina Redzepovic
Our country's healthcare system must prioritize Ranolazine education; it's a strategic asset in the fight against relentless angina that drains our workforce.
By mandating comprehensive counseling protocols across all cardiac centers, we reinforce national resilience and reduce costly emergency visits.
The pharmacodynamic profile-metabolic modulation without hemodynamic compromise-aligns perfectly with our goal of maintaining peak performance in the population.
Any laxity in patient instruction is a betrayal of national health security.
Esther Olabisi
Wow, another fancy drug and we’re supposed to read three pages of instructions 🙄.
Let’s just slap a colorful pill card on the fridge and hope they don’t forget, right? 🤷♀️
But seriously, a quick video walkthrough can turn that “meh” into a “yeah, I got this!” 🚀.
Rajesh Myadam
I appreciate the thorough breakdown; incorporating those teach‑back steps will definitely smooth the onboarding process.
Looking forward to seeing better adherence numbers across the board.