Learn which opioids are safe for kidney failure, how to adjust doses by GFR, and practical tips for monitoring side effects.
Safe Opioids for Kidney Disease: What You Need to Know
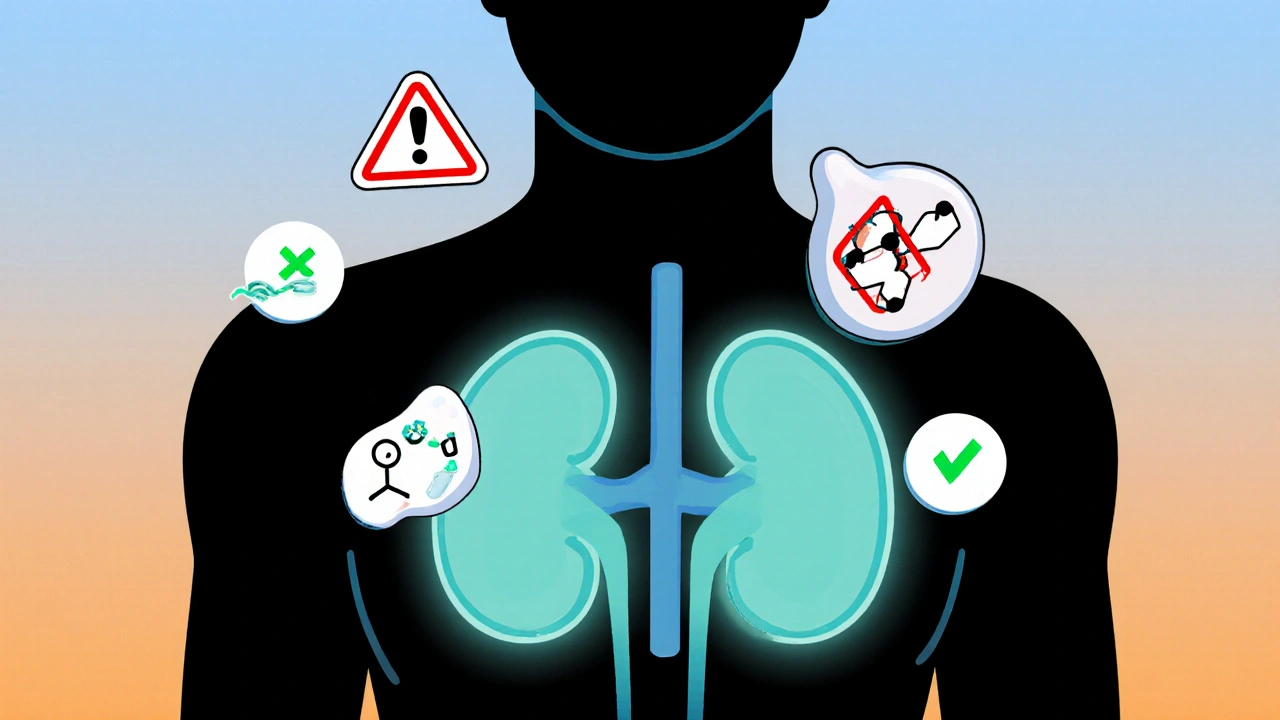
When you have kidney disease, a condition where the kidneys can’t filter waste properly, leading to buildup of toxins and fluid in the body. Also known as chronic kidney disease, it changes how your body handles many medications—including opioids. Not all painkillers are created equal here. Some opioids build up dangerously in people with reduced kidney function, while others are cleared safely even when kidneys are working at 30% capacity. The difference isn’t just about dosage—it’s about which drug you pick in the first place.
For someone with kidney disease, the real question isn’t just "Can I take opioids?" It’s "Which opioid won’t hurt me more than the pain?" Morphine, a common opioid used for severe pain, breaks down into compounds that stick around in the kidneys and can cause confusion, drowsiness, or even breathing trouble in advanced kidney disease. Hydromorphone, on the other hand, is metabolized differently and doesn’t produce the same toxic byproducts, making it a safer option for many patients. Fentanyl, a synthetic opioid used in patches or injections, is mostly broken down by the liver and doesn’t rely on kidney clearance, so it’s often preferred in late-stage kidney disease. You won’t find this info in most patient brochures. But if your kidneys are struggling, these details could keep you out of the ER.
It’s not just about picking the right opioid. It’s about timing, dose, and watching for side effects. People with kidney disease often need lower starting doses and longer gaps between doses. Even "safe" opioids can cause constipation, nausea, or dizziness—and those symptoms can get worse if you’re already feeling tired from dialysis or anemia. That’s why doctors who treat kidney patients often avoid long-acting opioids unless absolutely necessary. They prefer short-acting options they can adjust quickly. And they always check for interactions. If you’re also taking blood pressure meds, diuretics, or even over-the-counter painkillers like ibuprofen, your opioid risk goes up fast.
The posts below give you real, practical comparisons—what works, what doesn’t, and what to watch for. You’ll find clear breakdowns of opioid choices for kidney patients, how they’re dosed differently, and what alternatives—like nerve-targeting meds or physical therapies—can reduce opioid need. No fluff. No guesses. Just what matters when your kidneys are on the line.