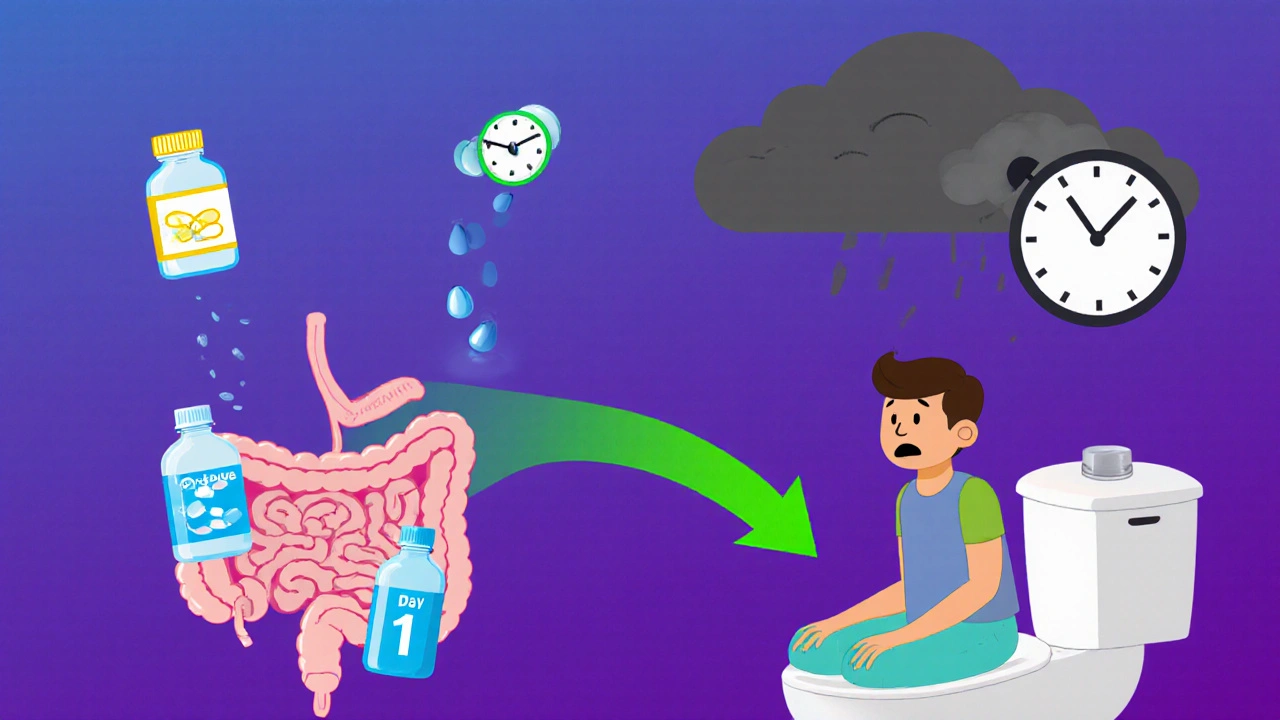
Opioid-induced constipation affects up to 60% of patients on long-term pain meds. Learn how to prevent it from day one and when to move beyond laxatives to prescription treatments like PAMORAs.
PAMORAs: What They Are, How They Work, and Why They Matter for Opioid Safety
When you take opioids for chronic pain, you’re not just fighting pain—you’re also fighting side effects like severe constipation, nausea, and bloating. That’s where PAMORAs, peripheral mu-opioid receptor antagonists that block opioid effects in the gut without affecting pain relief in the brain. Also known as peripherally acting mu-opioid receptor antagonists, these drugs let you keep the pain control you need while cutting out the gut misery. Unlike regular laxatives that just push things along, PAMORAs target the root cause: opioids binding to receptors in your intestines and slowing everything down.
PAMORAs like methylnaltrexone, naloxegol, and naldemedine are used when standard treatments fail. They’re not for everyone—usually prescribed to patients on long-term opioids for cancer pain, back issues, or arthritis. They’re also common in palliative care, where quality of life matters as much as pain control. These drugs don’t cross the blood-brain barrier, so they don’t undo the pain relief. That’s the whole point. They’re like a filter: blocking opioid chaos in the gut while leaving the brain alone. This makes them safer than switching opioids or reducing doses, which often leads to more pain or withdrawal.
But PAMORAs aren’t magic. They work best when paired with good hydration, fiber, and movement. Some patients still need stool softeners or enemas on top of them. And while they’re generally well-tolerated, side effects like abdominal pain or diarrhea can happen—especially if you’re not monitored. They’re also expensive, so insurance approval can be a hurdle. That’s why knowing which patients benefit most is key. If you’ve been on opioids for months and can’t have a normal bowel movement without help, PAMORAs might be the missing piece.
Looking at the posts here, you’ll find real-world examples of how PAMORAs fit into broader treatment plans. You’ll see how they connect to opioid dosing in kidney disease, how they relate to other gut-protecting drugs like PPIs, and how patient education makes or breaks their success. Whether you’re a patient tired of constipation or a provider trying to balance pain control with quality of life, the articles below give you the facts—no fluff, no jargon, just what works.