Opioid-Induced Constipation: How to Prevent and Treat It Effectively
Opioid Constipation Assessment Tool
What is the Bowel Function Index?
The Bowel Function Index (BFI) is a validated tool that measures constipation severity in patients taking opioids. It helps determine if your symptoms require prescription treatment. A score above 30 indicates severe constipation that typically needs stronger treatment options.
Your Bowel Function Index (BFI) Score
When you start taking opioids for chronic pain, you’re often warned about drowsiness, nausea, or the risk of dependence. But one of the most common and frustrating side effects? Constipation. In fact, opioid-induced constipation affects 40% to 60% of people taking these medications for non-cancer pain - and it doesn’t go away on its own. Unlike other side effects that fade over time, OIC sticks around as long as you’re on opioids. And if left untreated, it can lead to bloating, nausea, vomiting, and even bowel obstruction.
Why Opioids Cause Constipation
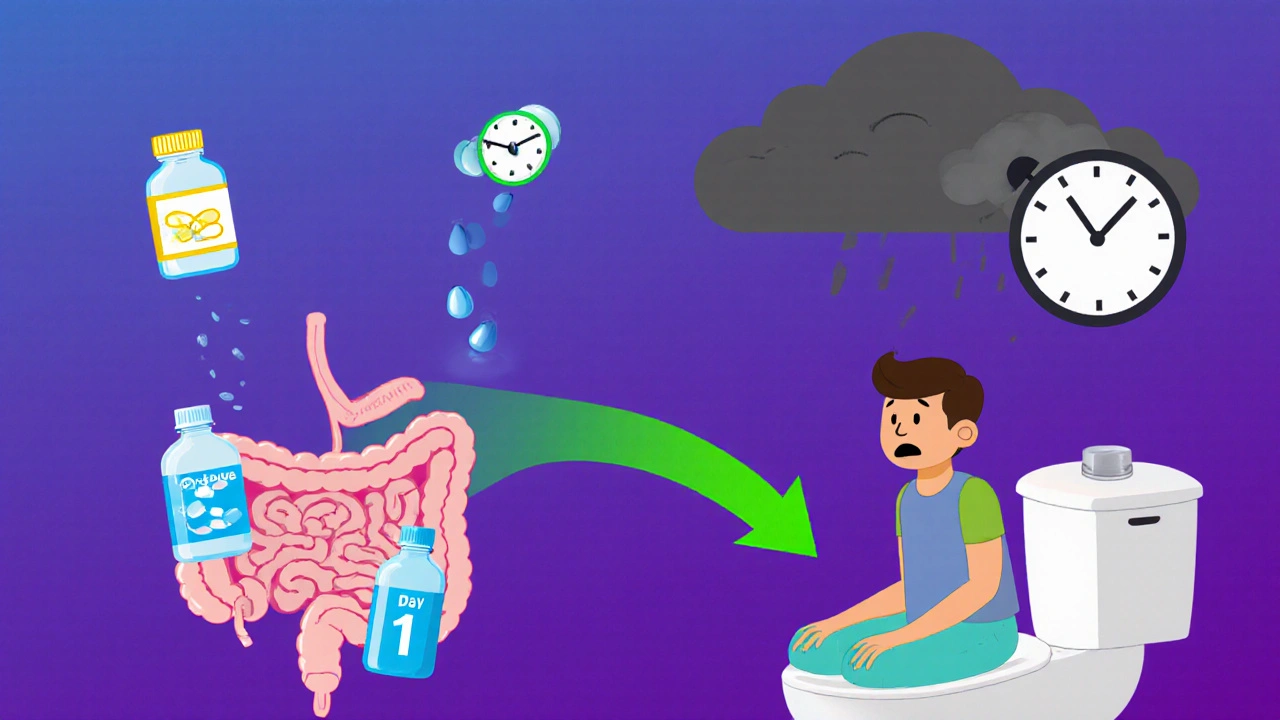
Opioids don’t just block pain signals in your brain. They also bind to receptors in your gut, specifically the μ-opioid receptors in the lining of your intestines. This slows down the natural muscle contractions that move food and waste through your digestive system. The result? Sluggish bowel movements, harder stools, and a feeling that you haven’t fully emptied your bowels - even after trying. It’s not just about slow movement. Opioids also increase the tone of your anal sphincter, making it harder to push out stool. And because your intestines absorb more water from waste, your stools become dry and compacted. This isn’t the same as occasional constipation from eating too little fiber. This is a drug-driven, persistent problem that doesn’t respond well to typical fixes like prunes or extra water.Prevention Starts on Day One
The biggest mistake people make? Waiting until they’re constipated to act. By then, it’s already a problem. Experts agree: if you’re starting opioids, you should start a laxative at the same time. Studies show that proactive treatment prevents 60% to 70% of severe cases. Your doctor or pharmacist should give you a plan before you even leave the clinic. The best first-line options are osmotic laxatives like polyethylene glycol (MiraLAX) or stimulant laxatives like senna. These work differently than fiber supplements, which often don’t help with OIC and can even make bloating worse. You also need to drink plenty of fluids - at least 2 liters a day - and stay active. Even a daily 20-minute walk helps keep things moving. But don’t rely on diet alone. No amount of broccoli or oatmeal will fully counteract the gut-slowing effects of opioids.What If Laxatives Don’t Work?
About 68% of patients report that over-the-counter laxatives aren’t enough. That’s when you need to move to prescription options called PAMORAs - peripherally acting μ-opioid receptor antagonists. These drugs block opioid receptors in your gut without crossing into your brain. That means they fix the constipation without taking away your pain relief. There are four main ones:- Methylnaltrexone (Relistor®): Given as an injection, it works in as little as 30 minutes. Often used in palliative care.
- Naldemedine (Symproic®): A daily pill. Shown to help not just with constipation, but also reduce opioid-induced nausea.
- Naloxegol (Movantik®): Another daily pill, approved for chronic non-cancer pain.
- Lubiprostone (Amitiza®): A chloride channel activator. Works well, but can cause nausea in up to 32% of users.

Who Should Avoid PAMORAs?
These drugs are powerful, but not safe for everyone. They’re contraindicated if you have a known or suspected bowel obstruction - which includes people with recent abdominal surgery, Crohn’s disease, or a history of intestinal blockages. There have been rare but serious cases of gastrointestinal perforation linked to PAMORAs, especially in people with weakened bowel walls. Patients with inflammatory bowel disease, recent surgery, or severe abdominal pain should be evaluated by a gastroenterologist before starting these medications. Your doctor should always check for signs of obstruction before prescribing them.Cost and Access Are Major Barriers
One of the biggest reasons people stop PAMORAs? Cost. A month’s supply can run $500 to $900 without insurance. Even with coverage, many plans require prior authorization or step therapy - meaning you have to try and fail on cheaper laxatives first. A 2023 survey found that 57% of patients discontinued PAMORAs within six months because of cost or lack of effectiveness. Medicare Part D plans require prior authorization for 41% of these drugs. Commercial insurers do it for 28%. If your insurance denies coverage, ask your doctor to file an appeal with clinical documentation showing failed laxatives and a Bowel Function Index (BFI) score above 30 - a validated tool that proves your constipation is severe enough to need stronger treatment.
Real Patient Experiences
On patient forums, stories are mixed. One user on HealthUnlocked wrote: “Relistor injections saved me. Nothing else worked - not even enemas.” Another on PatientsLikeMe said: “Naldemedine let me keep my pain meds without living in the bathroom.” But others report side effects: abdominal pain, diarrhea, or cramping. One Reddit user said: “I got relief, but the cramps were worse than the constipation.” And while some patients see dramatic improvement, others don’t respond at all. That’s why treatment isn’t one-size-fits-all. Sometimes you need to try two or three options before finding what works.What’s Next? The Future of OIC Treatment
The OIC treatment market is growing fast - projected to hit $2.1 billion by 2027. New developments are on the horizon. In 2023, a once-weekly injection of methylnaltrexone was approved, cutting down from daily shots to one per week. Researchers are also testing combination therapies - low-dose PAMORAs paired with mild laxatives - to boost effectiveness and reduce side effects. By 2026, experts predict personalized treatment based on genetic markers. Some people may naturally respond better to lubiprostone, while others benefit more from naldemedine. The American Society of Gastroenterology recently called for better insurance coverage, citing $2.3 billion in avoidable healthcare costs each year from untreated OIC complications like hospitalizations for fecal impaction.Bottom Line: Don’t Suffer in Silence
Opioid-induced constipation is common, persistent, and treatable - but only if you act early. Don’t wait for it to get bad. Start a laxative on day one of opioid therapy. Keep track of your bowel movements. If you’re straining, feeling full, or going less than three times a week, talk to your doctor. Don’t assume it’s just ‘normal’. PAMORAs are a game-changer for many, but they’re not magic. They require careful use, and access is still a hurdle. But with the right plan - proactive, personalized, and persistent - you can manage your pain without letting constipation take over your life.Is opioid-induced constipation the same as regular constipation?
No. Regular constipation is often caused by low fiber, dehydration, or inactivity. Opioid-induced constipation (OIC) is caused by drugs binding to receptors in your gut, slowing movement and hardening stool. It doesn’t respond well to fiber or lifestyle changes alone and usually needs specific laxatives or PAMORAs.
Can I just use MiralAX or senna forever?
Many people do - and it’s often the first step. But studies show that up to 68% of patients on long-term opioids don’t get enough relief from over-the-counter laxatives. If you’re still struggling after 2-4 weeks, it’s time to talk to your doctor about PAMORAs. Long-term use of stimulant laxatives can lead to dependency or electrolyte imbalances.
Do PAMORAs reduce my pain relief?
No. PAMORAs are designed to block opioid receptors only in the gut, not in the brain. That means they fix constipation without interfering with pain control. Clinical trials confirm that patients maintain their pain relief while improving bowel function.
Why do some people say PAMORAs cause stomach pain?
PAMORAs speed up gut movement, which can cause cramping or diarrhea, especially at first. Naloxegol and methylnaltrexone are more likely to cause abdominal pain than naldemedine. Starting with a lower dose or taking it with food can help. If pain is severe or persistent, contact your doctor - it could signal a more serious issue.
Is there a way to avoid OIC without taking more pills?
Not reliably. While hydration, movement, and fiber help, they’re not enough on their own. OIC is a direct pharmacological effect. The most effective approach is combining lifestyle changes with a proven laxative from day one. Avoiding opioids isn’t always an option for chronic pain patients - so managing the side effect is essential.
How do I know if I need a PAMORA?
If you’ve been using laxatives for 2-4 weeks and still have fewer than three bowel movements per week, or if you’re straining, feeling bloated, or having incomplete evacuations, it’s time to consider escalation. Doctors use the Bowel Function Index (BFI) - a simple 3-question tool. A score above 30 means significant constipation that likely needs prescription treatment.
Can I switch from one PAMORA to another if it doesn’t work?
Yes. Not everyone responds to the same drug. If naldemedine doesn’t help after 4 weeks, your doctor might try naloxegol or methylnaltrexone. Some patients respond better to injections, others to pills. It’s trial and error - but there are options. Don’t give up after one try.

Stuart Rolland
Okay, I’ve been on opioids for three years now, and let me tell you - this post is the first thing that actually made sense. I thought I was just lazy or not drinking enough water. Turns out, my gut was basically on vacation while I was trying to function. Started MiraLAX on day one after my doc told me to, and honestly? Saved my life. No more bloating at work, no more panic attacks before leaving the house. Just a quiet, normal bowel movement. If you’re reading this and you’re on opioids - don’t wait. Start the laxative. TODAY. Your future self will thank you.
Also, walks. Even 10 minutes. Just move. Your colon isn’t a magic box - it needs motion. I started walking after dinner, no phone, just me and the sidewalk. It’s weirdly meditative. And yeah, it works.
Charlos Thompson
Oh wow. So instead of just telling people to ‘eat more fiber,’ we now have a $900/month pill that ‘blocks opioid receptors in the gut but not the brain’ - like that’s some kind of sci-fi magic bullet. Next up: a $1,200 supplement that tells your liver to ‘please don’t metabolize pain meds so aggressively.’
Meanwhile, my grandma pooped once a week on prune juice and still lived to 98. Maybe we just need to stop treating constipation like a villain in a Marvel movie and start treating it like… a normal human problem?
Jessica Glass
Let me get this straight - you’re telling me people are getting prescribed opioids for ‘chronic pain’ and then acting shocked when their digestive system shuts down like a Windows 95 computer? This isn’t a medical mystery. This is what happens when you treat pain like a video game boss you just need a better weapon for.
And now we’re giving people $900/month pills so they can keep taking the drug that broke them in the first place? Brilliant. Just brilliant. Next up: a pill to un-break your spine after you took the painkiller that made you numb to everything - including consequences.
Rohit Nair
Hi, I’m from India and my dad is on opioids for spinal pain. We tried everything - psyllium, dates, warm water in morning, yoga, even ayurvedic laxatives. Nothing worked. Then the doctor gave him naldemedine. First day, he said he felt like a 20-year-old again. No cramps, no nausea, just… normal. Cost was high, but we got it through a patient assistance program. I wish more doctors here knew about this. Most still say ‘eat more dal and spinach.’ Lol. This post is gold. Thank you.
Lilly Dillon
I’ve been on methylnaltrexone injections for a year. I used to dread weekends because I’d be stuck on the toilet for hours. Now? I go out. I travel. I don’t think about it anymore. It’s not perfect - the injection site stings, and sometimes I get diarrhea. But it’s the difference between living and just existing. If you’re struggling, don’t feel guilty for asking for help. Your body deserves relief.
Richard Kang
Okay so I tried MiraLAX, then senna, then a colon cleanse (yes, really), then I started drinking kombucha like it was water, and then I bought one of those vibrating belly belts on Amazon - and guess what? NOTHING. I was literally crying in the bathroom one night because I hadn’t gone in 5 days and my stomach looked like I was 7 months pregnant. Then my nurse practitioner said ‘try Relistor.’ I was like ‘is that a new TikTok trend?’ She said ‘no, it’s an injection.’ I cried again - but this time because it worked in 45 minutes. I’m not even mad anymore. Just grateful. And yes, I still have to inject myself like a vampire with a bad attitude. But I’d rather be a vampire than a human brick.
Gavin McMurdo
Let’s be honest - the entire opioid system is a corporate-engineered trap. You’re given a drug that causes a side effect, then sold a more expensive drug to fix it, then charged a premium for insurance paperwork, and then blamed for not being ‘compliant’ when you can’t afford the solution. This isn’t medicine. It’s a business model disguised as healthcare.
And yet, here we are, praising PAMORAs like they’re the second coming, while ignoring the fact that we could’ve avoided this entire mess if we’d treated pain with physical therapy, acupuncture, or - gasp - less reliance on narcotics in the first place.
But no. Let’s just keep the pipeline flowing. More pills. More injections. More bills. More despair.
Krishna Kranthi
My cousin in Delhi got prescribed opioids after a car accident. He tried everything - even tried yoga with a yoga ball and drank warm milk with ghee. Nothing. Then his doctor in Mumbai told him about naloxegol. He was skeptical. But after 2 weeks? He said he could finally sit on the floor to eat without feeling like his intestines were made of concrete.
Cost? 30k INR/month. Crazy. But he got it through a hospital program. I told him - if you can get this, you’re lucky. Most people here just suffer. Or worse - stop the pain meds. And then the pain comes back harder.
So yeah. This post? Spot on. But it needs to reach more people. Not just in the US. In India. In Nigeria. In Peru. This is global.
Jesse Weinberger
Wait so you’re telling me that the same drug that kills your gut is also the only thing keeping your pain down? And instead of fixing the root problem - like finding non-opioid pain management - we just keep slapping more pills on top? Classic American healthcare. Fix the symptom, ignore the cause, charge $800 for a pill that’s been around since 2012.
Also, why is everyone acting like PAMORAs are some revolutionary breakthrough? They’ve been in trials since the 2000s. We just didn’t care until Big Pharma found a way to monetize constipation.
And don’t even get me started on ‘Bowel Function Index.’ Sounds like something a robot wrote after watching 17 episodes of Grey’s Anatomy.
Shiv Sivaguru
So basically you’re saying if you’re on opioids you need to spend $900 a month to poop? And if you can’t afford it, you just… stop? And then your pain comes back? And then you’re stuck between agony and impaction? That’s not healthcare. That’s a hostage situation.
Also, why is no one talking about the fact that most of these drugs were developed because of lobbying? Not science. Not patient need. Just profit.
I’m not even mad. I’m just… tired.
Wendy Stanford
There’s a quiet horror in how normalized this has become. We don’t talk about the fact that opioids turn your body into a prison. Your mind is numb, your gut is frozen, your dignity is buried under layers of stool and shame. And instead of asking why we’re prescribing these drugs so freely - we just hand out prescriptions for more prescriptions.
I’ve seen people cry because they couldn’t go to their child’s school play because they were too bloated. I’ve seen husbands avoid intimacy because they were too embarrassed. This isn’t just constipation. It’s a slow erosion of personhood.
And we call it ‘side effect.’
That word. That tiny, flippant word. It hides a world of suffering.
Maybe we need to stop calling it OIC and start calling it what it is - the price of pain relief.
Peter Feldges
While I appreciate the clinical thoroughness of this post, I must respectfully observe that the implicit assumption - that opioid therapy is an acceptable long-term solution for non-cancer chronic pain - remains largely uninterrogated. The data presented on PAMORA efficacy, while statistically significant, fails to contextualize the broader ethical implications of pharmaceutical dependency cascades. One might posit that the true innovation lies not in pharmacological countermeasures, but in systemic reevaluation of pain management paradigms. That said, I commend the inclusion of BFI metrics; their validation offers a measurable, patient-centered outcome parameter previously absent from clinical discourse. A minor typo, however: ‘lubiprostone’ is misspelled as ‘lubiprostone’ in the third paragraph. Please correct for scholarly integrity.
Stuart Rolland
Re: @Peter Feldges - I love that you said ‘systemic reevaluation.’ But here’s the thing - for a lot of us, there’s no ‘other option.’ I have spinal stenosis. I can’t walk more than 10 minutes without my legs going numb. Physical therapy? Tried it. Acupuncture? Tried it. Nerve blocks? Tried it. They all failed. Opioids are the only thing that lets me hold my daughter without screaming.
So yeah - maybe the system is broken. But I’m not asking for a revolution. I’m asking for a pill that lets me poop.
And if that pill costs $900? Fine. But don’t make me beg for it. Don’t make me jump through 17 insurance hoops. Just let me live.