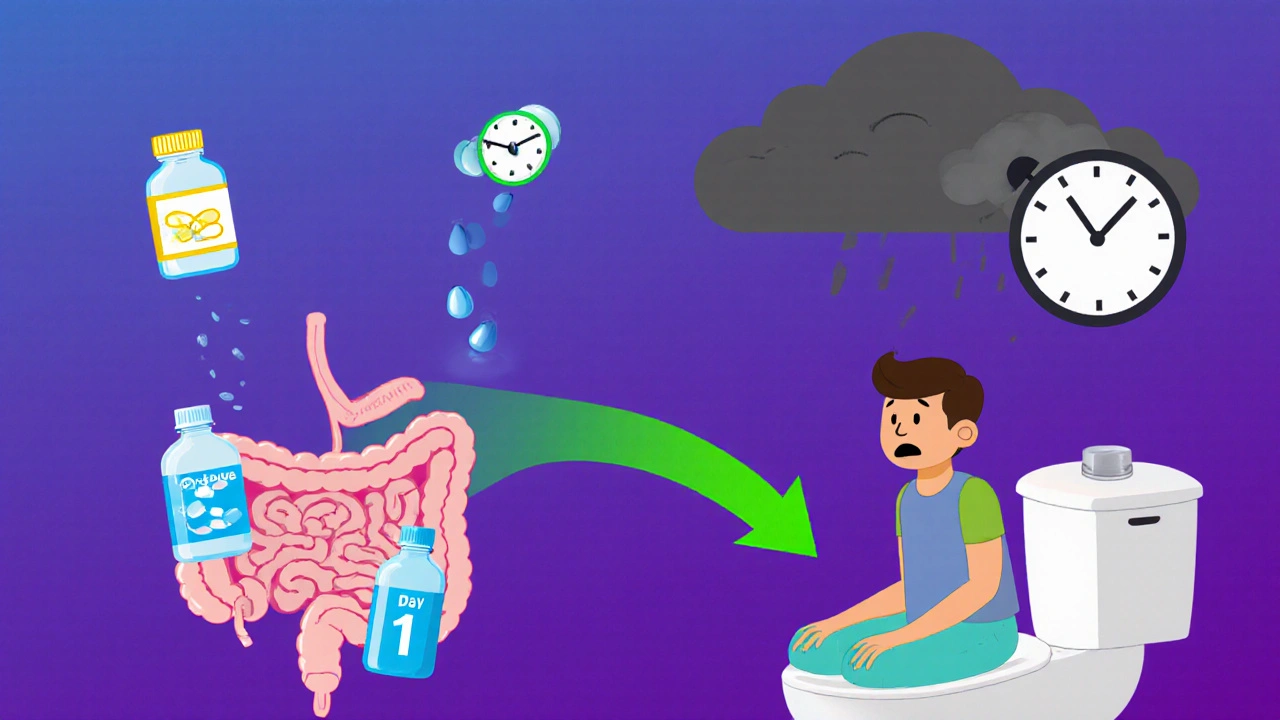
Opioid-induced constipation affects up to 60% of patients on long-term pain meds. Learn how to prevent it from day one and when to move beyond laxatives to prescription treatments like PAMORAs.
Opioid-Induced Constipation: Causes, Solutions, and What Works
When you take opioids for chronic pain, opioid-induced constipation, a side effect caused by opioids slowing down the digestive tract. It’s not just discomfort—it’s a real problem that can make you skip doses or quit pain meds altogether. Also known as opioid bowel dysfunction, it happens because these drugs bind to receptors in your gut, reducing muscle movement and fluid secretion. Unlike regular constipation, it doesn’t get better with more fiber or water alone. About 80% of people on long-term opioids deal with it, and most doctors don’t talk about it unless you bring it up.
This isn’t just about going to the bathroom less. It’s about bloating, nausea, feeling full all the time, and even vomiting. And if you’re on opioids because of kidney disease or heart failure, you’re even more at risk—your body handles drugs differently. That’s why some posts here focus on safe opioids for kidney failure, specific drugs like fentanyl or buprenorphine that are less likely to worsen gut function. Others look at proton pump inhibitors, used for acid reflux but sometimes misused as a fix for opioid gut issues, even though they don’t touch the real problem. You need something that moves things along in your intestines, not just reduces stomach acid.
The good news? There are proven fixes. Laxatives like polyethylene glycol or stimulant laxatives (senna) help, but newer options like methylnaltrexone or naloxegol target only the gut, leaving pain relief intact. Some people find relief with daily movement, hydration, or even probiotics—but these work best alongside targeted meds. What doesn’t work? Just eating more fiber. What’s dangerous? Ignoring it until you develop a bowel obstruction. The posts below cover real strategies: which laxatives to try first, how to talk to your doctor about switching opioids, what to avoid when you’re also on heart or kidney meds, and how to track your symptoms so you don’t just suffer in silence.
You’re not alone in this. Millions of people manage pain with opioids and still need to stay regular. The right approach doesn’t mean giving up your meds—it means fixing the side effect without compromising your relief. Below, you’ll find practical guides from real patients and clinicians who’ve been there. No fluff. No theory. Just what helps—and what doesn’t.