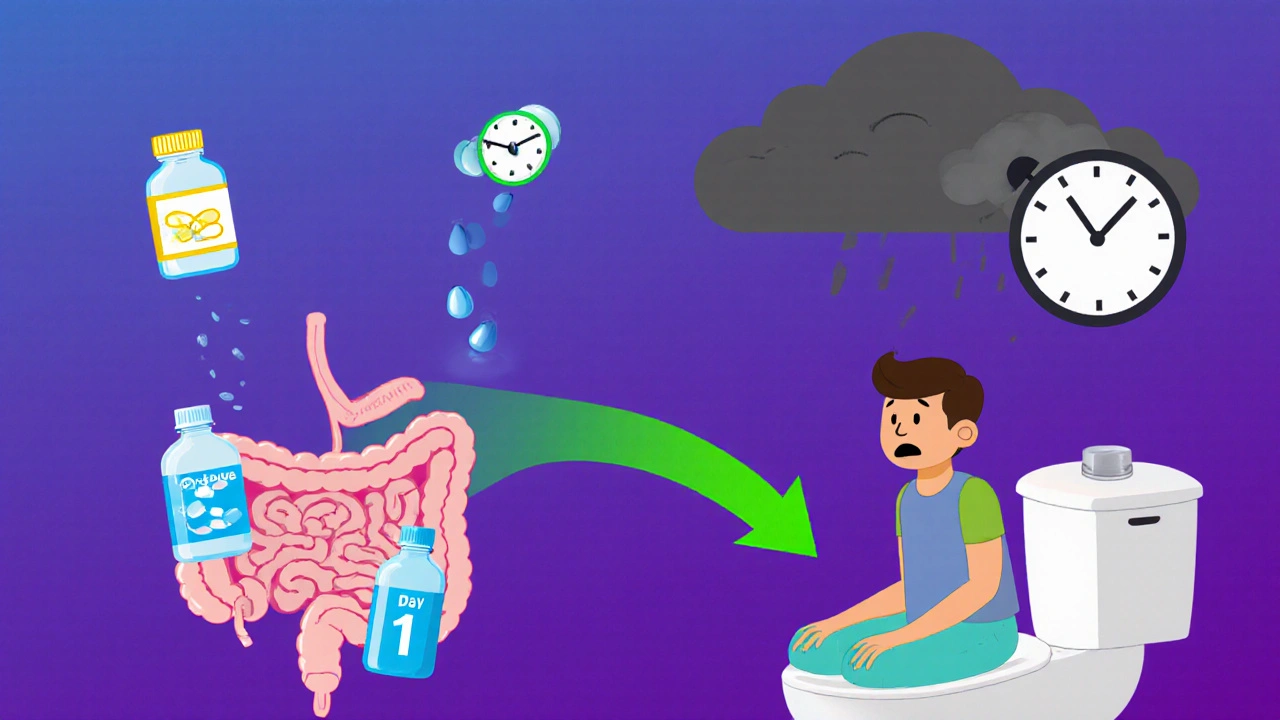
Opioid-induced constipation affects up to 60% of patients on long-term pain meds. Learn how to prevent it from day one and when to move beyond laxatives to prescription treatments like PAMORAs.
OIC Treatment: Safe Options, Common Drugs, and What Works Best
When you’re taking opioids for pain, OIC treatment, the management of opioid-induced constipation, a common and often overlooked side effect of long-term opioid use. Also known as opioid-induced constipation, it’s not just discomfort—it can make you stop taking pain meds altogether, or worse, lead to bowel blockages. This isn’t rare. Up to 80% of people on long-term opioids deal with it, and most over-the-counter laxatives barely touch it.
That’s why naloxegol, a peripherally acting mu-opioid receptor antagonist specifically designed to relieve constipation without affecting pain control and methylnaltrexone, an injectable or oral drug that blocks opioid effects in the gut while leaving brain pain relief intact exist. They’re not magic, but they work where traditional laxatives fail. You won’t find them on every pharmacy shelf, but they’re prescribed when senna, polyethylene glycol, or stool softeners don’t cut it. These drugs target the root cause: opioids slowing down your gut. They don’t just push— they restore normal movement.
But here’s the thing: OIC treatment isn’t just about pills. It’s about timing, diet, and movement. Drinking more water helps, but only if you’re not already dehydrated from other meds. Moving your body—even walking 20 minutes a day—can kickstart your bowels better than some drugs. And if you’re on multiple pain meds, like fentanyl or oxycodone, your OIC risk goes up fast. That’s why doctors now check for constipation at every visit, not just when you complain. It’s part of the treatment plan, not an afterthought.
What you’ll find below are real, practical guides that cut through the noise. From how to pick the right laxative without worsening nausea, to why some patients do better on naloxegol than methylnaltrexone, and how to talk to your doctor about switching pain meds without losing control. These aren’t theory pieces. They’re written by people who’ve been there—patients who fought through constipation while managing chronic pain, and clinicians who’ve seen what actually works in the real world. No fluff. No guesswork. Just what helps, what doesn’t, and how to get there safely.