Hypoparathyroidism: How to Manage Low Calcium and Vitamin D Effectively
When your parathyroid glands don’t make enough hormone, your body can’t keep calcium in check. That’s hypoparathyroidism. It’s rare, but if you’ve had thyroid surgery, have an autoimmune condition, or were born with a genetic issue like DiGeorge syndrome, you’re at risk. The result? Low calcium, high phosphate, and symptoms like tingling fingers, muscle cramps, fatigue, or even seizures if left untreated. The good news? You can manage it. But it’s not simple. It takes precision, patience, and a clear plan.
Why Calcium and Vitamin D Are Non-Negotiable
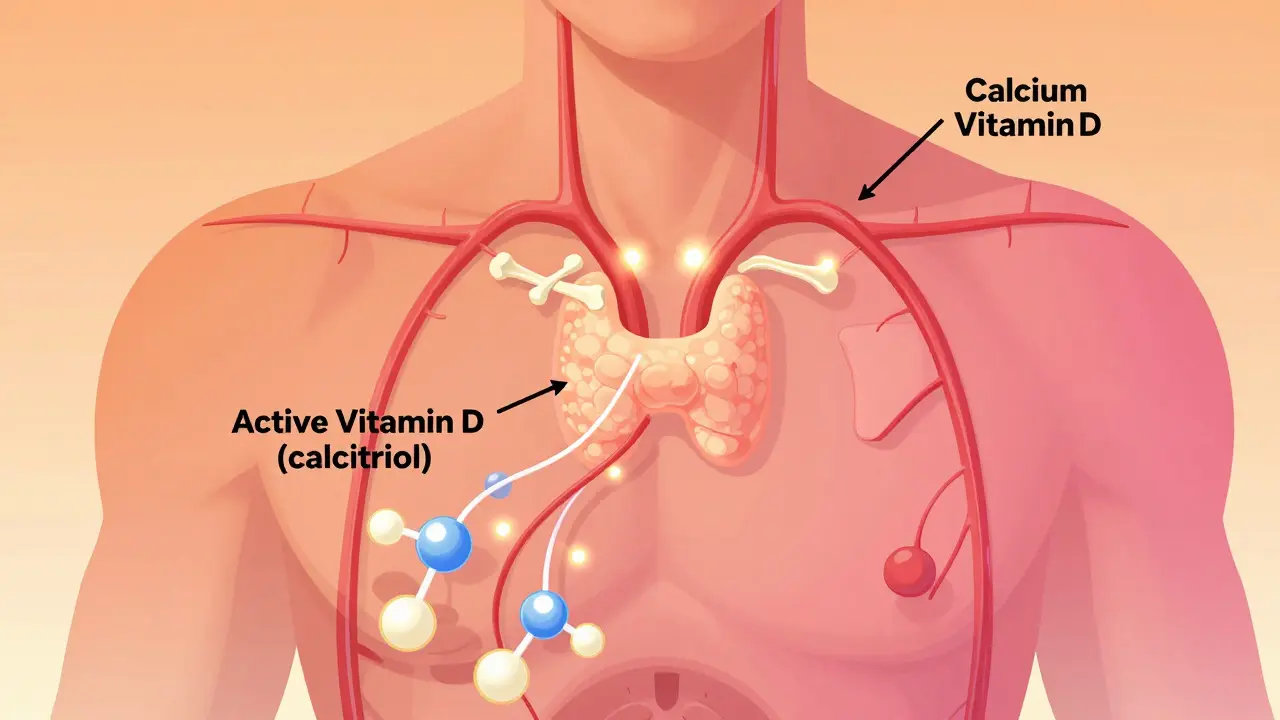
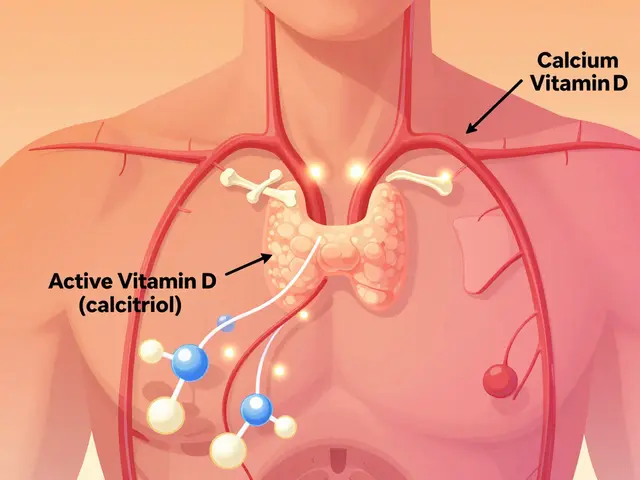
Without parathyroid hormone (PTH), your body can’t pull calcium from your bones or absorb it from food. Your kidneys also can’t recycle calcium properly. So, your blood calcium drops. That’s dangerous. Your nerves, muscles, and heart rely on stable calcium levels. If it dips too low, you get numbness around the mouth, hand spasms, or heart rhythm problems.
Vitamin D isn’t just for bones here. In hypoparathyroidism, your body can’t convert regular vitamin D (D3) into its active form because PTH is missing. That’s why you need active vitamin D analogues - calcitriol or alfacalcidol. These bypass the broken step. They work directly. Regular vitamin D supplements won’t cut it. Studies show calcitriol raises calcium levels 2.3 times faster than D3 alone.
What Your Dosing Should Look Like
There’s no one-size-fits-all dose, but here’s what most experts follow based on guidelines from Parathyroid UK, the European Society of Endocrinology, and the Mayo Clinic.
Calcium: Start with 1,000 to 2,000 mg daily, split into two or three doses. Take it with meals. Why? Food helps absorption, and calcium also acts as a phosphate binder - it grabs excess phosphate in your gut before it enters your blood. Calcium carbonate is the go-to form. It’s cheap and packs 40% elemental calcium. So, if you need 1,000 mg of elemental calcium, you take 2,500 mg of calcium carbonate. Calcium citrate? Less efficient - you’d need almost twice as much.
Active Vitamin D: Begin with 0.25 to 0.5 mcg of calcitriol or alfacalcidol daily. Some need more, some need less. Your doctor will adjust based on blood tests. Never skip this. Without it, calcium supplements won’t work.
Regular Vitamin D3: Even if you’re on active D, you still need 400-800 IU of vitamin D3 daily. This keeps your overall vitamin D stores at 20-30 ng/mL. Low stores can make your body less responsive to treatment.
Monitoring Is Everything
Checking your blood once a year won’t cut it. In the first few months, you’ll need blood tests every 1-3 months. Once stable, every 4-6 months is typical. But here’s what you must track:
- Serum calcium: Aim for 2.00-2.25 mmol/L (8.0-8.5 mg/dL). Not higher. Going above 2.35 mmol/L increases your risk of calcium deposits in your brain, kidneys, and blood vessels.
- 24-hour urinary calcium: This is critical. You want less than 250 mg per day. Too much? You’re at risk for kidney stones - 5 to 7 times more likely if you’re not monitoring this.
- Serum phosphate: Keep it between 2.5-4.5 mg/dL. High phosphate makes calcium harder to control.
- Magnesium: If it’s below 1.7 mg/dL, your body can’t use calcium or vitamin D properly. Supplement with magnesium oxide or citrate - 400-800 mg daily if needed.
Many patients don’t realize that a single high calcium reading can mean trouble. It’s not just about feeling okay. You need the numbers to stay in the safe zone long-term.
Dietary Rules You Can’t Ignore
Food matters. Not as much as medication, but it’s a tool.
Do eat: Dairy (milk, yogurt - 300 mg calcium per serving), kale (100 mg per cup), broccoli (43 mg per cup), fortified plant milks, and canned fish with bones like sardines.
Avoid or limit: Soda (one liter has 500 mg phosphorus), processed meats (150-300 mg per serving), hard cheeses (500 mg per ounce), and packaged snacks. These spike phosphate, which pulls calcium out of your blood and into your tissues - where it doesn’t belong.
Also, keep sodium under 2,000 mg daily. High salt makes your kidneys dump more calcium into urine. If you’re struggling with high urinary calcium, cutting salt can help more than adding more meds.

When Standard Treatment Isn’t Enough
About 25-30% of people can’t get stable with calcium and vitamin D alone. You might be one of them if:
- You need more than 2,000 mg of calcium daily
- You need more than 2 mcg of active vitamin D daily
- You still have high urinary calcium despite max doses
- You’re constantly tired, tingling, or anxious - even with "normal" blood levels
Then it’s time to talk about PTH replacement. There are two options: Natpara (recombinant human PTH 1-84) and Forteo (teriparatide, PTH 1-34). Both are daily injections. Natpara is approved in the UK and EU, though it’s expensive - around £1,200 a month. Forteo is cheaper but not officially approved for hypoparathyroidism, so it’s off-label.
Studies show PTH therapy reduces calcium and vitamin D needs by 30-40%. It also lowers urinary calcium, which protects your kidneys. But it’s not for everyone. You need to be comfortable with injections, have good insurance, and be willing to go through a strict monitoring program.
The Hidden Problem: Magnesium and the "Calcium Rollercoaster"
Many patients don’t know magnesium is part of the puzzle. Low magnesium = low calcium, even if you’re taking tons of calcium. That’s because magnesium is needed for PTH to work - and even for your cells to respond to calcium.
One patient from Manchester, who’d been on treatment for 8 years, told me: "I felt fine until I realized I was only taking calcium in the morning and at night. I’d get shaky by 3 p.m." Switching to four smaller doses - breakfast, lunch, snack, dinner - made her stable. That’s the "calcium rollercoaster" so many describe: highs and lows that cause fatigue, brain fog, or panic attacks.
Splitting your doses - even five times a day - helps. And keeping magnesium above 1.9 mg/dL cuts hypocalcemic episodes by 35%, according to a Cleveland Clinic study.
What About New Treatments?
There’s hope on the horizon. TransCon PTH is a once-daily injection that slowly releases PTH. In a 2022 trial, 89% of patients kept calcium normal without calcium or vitamin D supplements. That’s huge. It’s not available yet, but phase 3 trials are complete. It could be approved by 2026.
Gene therapy is also being studied - targeting the calcium-sensing receptor to trick the body into thinking calcium is normal. But that’s still years away.
Living With It: Real Tips for Daily Life
- Always carry calcium tablets. If you feel tingling or cramping, chew 2-3 tablets (500-1,000 mg elemental calcium) right away.
- Take vitamin D at bedtime. It absorbs better when your stomach is empty.
- Use a pill organizer. You might be taking 6-10 pills a day. Missing one can throw you off.
- Get a medical ID bracelet. If you collapse, paramedics need to know you’re on calcium therapy.
- Join a patient group. The Hypopara Alliance and Reddit’s r/Hypoparathyroidism have thousands of people sharing real-life tricks - like which brands of calcium work best, how to get insurance to cover Natpara, or how to handle travel with meds.
Most importantly, don’t settle for "close enough." If you’re still having symptoms, your levels aren’t truly stable. Push for better control. Your kidneys, your brain, and your quality of life depend on it.
Who Should Manage Your Care?
Start with an endocrinologist. They’ll handle the first 3-4 months of dose tweaks. Once stable, your GP can take over - if they’re trained. But here’s the problem: 78% of family doctors say they don’t feel confident managing hypoparathyroidism. So, keep your endocrinologist on speed dial. Even stable patients should see them once or twice a year.
Don’t let a busy schedule delay your tests. A single missed urine test could mean you’re slowly damaging your kidneys without knowing it.
Can I stop taking calcium if I feel fine?
No. Even if you feel fine, low calcium can quietly damage your kidneys, heart, and brain over time. Hypoparathyroidism requires lifelong treatment. Stopping calcium or vitamin D can lead to severe symptoms like seizures or heart arrhythmias within hours.
Why not just take more vitamin D3 instead of calcitriol?
Your body needs PTH to convert vitamin D3 into its active form. In hypoparathyroidism, that conversion doesn’t happen. Taking more D3 won’t help - it just builds up unused in your liver. Calcitriol is already active. It works directly, bypassing the broken step. Studies show it’s 2.3 times faster and more effective.
Is it safe to take calcium and vitamin D long-term?
Yes - if you’re monitored. The real danger isn’t the supplements themselves, but uncontrolled calcium levels. Taking too much calcium without checking urinary calcium raises kidney stone risk by 5-7 times. That’s why regular 24-hour urine tests are essential. When managed properly, long-term use is safe and life-saving.
Can I get PTH replacement therapy on the NHS?
Natpara is approved in the UK and available on the NHS for patients who meet specific criteria - usually those needing high-dose calcium or vitamin D, or those with persistent hypercalciuria. Access can be slow due to cost and prior authorization. Talk to your endocrinologist about applying through the Specialised Commissioning pathway.
What’s the biggest mistake people make with hypoparathyroidism?
Waiting until they feel bad to check their levels. Many patients only test when symptoms flare. But damage builds silently. The goal isn’t to feel okay - it’s to keep calcium in the narrow safe zone (2.00-2.25 mmol/L) every single day. Regular blood and urine tests prevent long-term kidney and brain damage.
Should I avoid dairy because it has phosphorus?
No. Dairy is one of the best sources of calcium. The key is balance. Avoid processed foods with added phosphorus - soda, deli meats, frozen meals. But whole milk, yogurt, and cheese in moderation are fine. Pair them with calcium-binding meals and monitor your phosphate levels. Cutting dairy often makes calcium harder to control.
Can magnesium supplements help with muscle cramps?
Yes - if your magnesium is low. Muscle cramps in hypoparathyroidism are often caused by low calcium, but low magnesium makes it worse. If your blood magnesium is below 1.7 mg/dL, supplementing can reduce cramps and improve how your body uses calcium. Don’t guess - get tested first.
Final Thought: It’s Manageable, But It Demands Attention
Hypoparathyroidism isn’t curable yet. But it’s controllable. You don’t need to live in fear of tingling hands or muscle spasms. With the right mix of calcium, active vitamin D, magnesium, diet, and monitoring, you can live a full, stable life. The trick is consistency. Not perfection. Just showing up - for your blood tests, your pills, your meals. The numbers will follow.

Scott Butler
This post is pure gold. Finally someone who gets it. No more "just take vitamin D" nonsense from quacks. Calcitriol isn't optional-it's the only thing keeping me off the ICU. If you're still using D3 alone, you're playing Russian roulette with your heart.
And don't even get me started on magnesium. I was cramping like a damn cowboy until I hit 600mg daily. Now I sleep through the night. Stop guessing. Test your levels.
Also, Natpara? It's a godsend. Why the NHS makes you jump through hoops for it is beyond me. This isn't a luxury-it's medical necessity.
Emma Sbarge
I've been on this regimen for 12 years. Calcium carbonate 2,500mg three times a day. Calcitriol 0.5mcg. Magnesium 400mg. No soda. No processed junk. And yes, I still get the tingles sometimes. But I'm alive. That's more than I can say for some people who thought they could wing it.
Don't listen to the internet gurus who say "you don't need meds if you eat kale." You do. Always.
Deborah Andrich
Thank you for writing this with such clarity. I wish I'd had this when I was first diagnosed. I spent two years going from doctor to doctor, told I was "just anxious," until my hands locked up during a meeting and I ended up in the ER.
Splitting doses saved me too. I used to take all my calcium in the morning and crash by 2pm. Now I spread it out like clockwork-breakfast, lunch, snack, dinner. No more brain fog. No more panic attacks.
And yes, magnesium. I didn't know it mattered until my endo tested me. Low magnesium is silent, but it's stealing your stability.
You're not alone. Keep showing up. Even on the days you feel fine. That's the real win.
Aman deep
bro this is lit 😅
i was on d3 for 3 years thinkin it was enough then my doc said "you're not making pth so d3 is just sitting there like a decoration" and i was like... oh. right.
calcitriol changed my life. no more cramps at 3am. no more numb fingers when i text.
also magnesium 600mg daily. i use citrate. no more leg cramps like i'm in a western movie.
and yes i carry calcium tabs like candy. one time i felt tingling in the subway and chewed two tabs. no one knew. i just looked like i was chewing gum.
ps: transcon pth is gonna be a game changer. cant wait. i'll be first in line.
Eddie Bennett
Been here for 8 years. I used to think if I felt okay, I was fine. Big mistake. My kidneys started showing damage before I felt a thing.
24-hour urine test? Non-negotiable. I missed one for six months. Turned out I was peeing out 420mg of calcium. Scary.
Now I do it every 4 months like clockwork. My doc says my numbers are the cleanest he's seen in a long time.
Also-yes, dairy is fine. I drink a glass of milk every night. No guilt. No fear. Just balance.
And if you're thinking about skipping meds because you "feel fine"-don't. Your body doesn't lie. The numbers do.
Sylvia Frenzel
So let me get this straight-you're telling me the government won't cover Natpara unless you're "desperate"? But they'll pay for a $20,000 cancer drug that gives you 3 extra months?
Of course. Because this is a "rare disorder." And we all know what happens to rare disorders. They get ignored until someone dies.
I'm not mad. I'm just... disappointed. This isn't science. This is politics. And we're the collateral damage.
Constantine Vigderman
OMG YES!! I just started calcitriol last month and my energy is back!! I used to nap after lunch like I was 80. Now I’m hiking on weekends. 🙌
Also-magnesium changed EVERYTHING. I was skeptical but my cramps vanished. I take it with dinner now. Best decision ever.
And YES carry calcium! I keep a little bottle in my purse, my car, my gym bag. One time I got tingling in the grocery store and popped two tabs. No one noticed. I just looked like I was eating a mint.
Also-transcon pth is coming? I’m already pre-ordering my injection pen. This is the future!! 💪
Tyrone Marshall
There’s a quiet dignity in managing this condition. It’s not glamorous. You don’t get trophies for taking pills at 7am, 12pm, 5pm, and 9pm. No one sees the 24-hour urine collection jars in your bathroom. No one applauds when your calcium stays in range for six months straight.
But you’re doing something profound: you’re choosing life, day after day, when no one’s watching.
That’s not weakness. That’s courage.
And if you’re reading this and feeling tired of the routine? You’re not failing. You’re still in the game. And that’s everything.
Emily Haworth
Wait… so you’re saying this isn’t a vaccine side effect? 🤔
I read somewhere that Big Pharma is hiding the truth about parathyroid damage from mRNA shots. That’s why so many people are getting hypoparathyroidism now. They don’t want you to know.
Also, I heard the government is putting fluoride in the water to lower calcium levels so people become dependent on calcitriol. That’s why they won’t cover Natpara-it’s too effective.
My cousin’s neighbor’s dog got it after a rabies shot. Coincidence? I think not. 🚨
Someone needs to investigate this. I’m starting a petition.
Tom Zerkoff
Thank you for the comprehensive and clinically accurate overview. The integration of evidence-based dosing parameters, metabolic physiology, and patient-centered management strategies is exemplary.
Of particular note is the emphasis on 24-hour urinary calcium monitoring as a primary endpoint for renal protection-a metric frequently underutilized in primary care settings. The distinction between calcium carbonate and citrate, the rationale for active vitamin D analogues, and the role of magnesium in cellular responsiveness are all articulated with precision.
It is imperative that this information be disseminated to endocrinology trainees and primary care providers alike, given the documented gap in clinical confidence among general practitioners.
Further research into the long-term renal outcomes of patients on PTH replacement therapy remains a critical unmet need. I look forward to the forthcoming phase 3 data on TransCon PTH.
Well done.