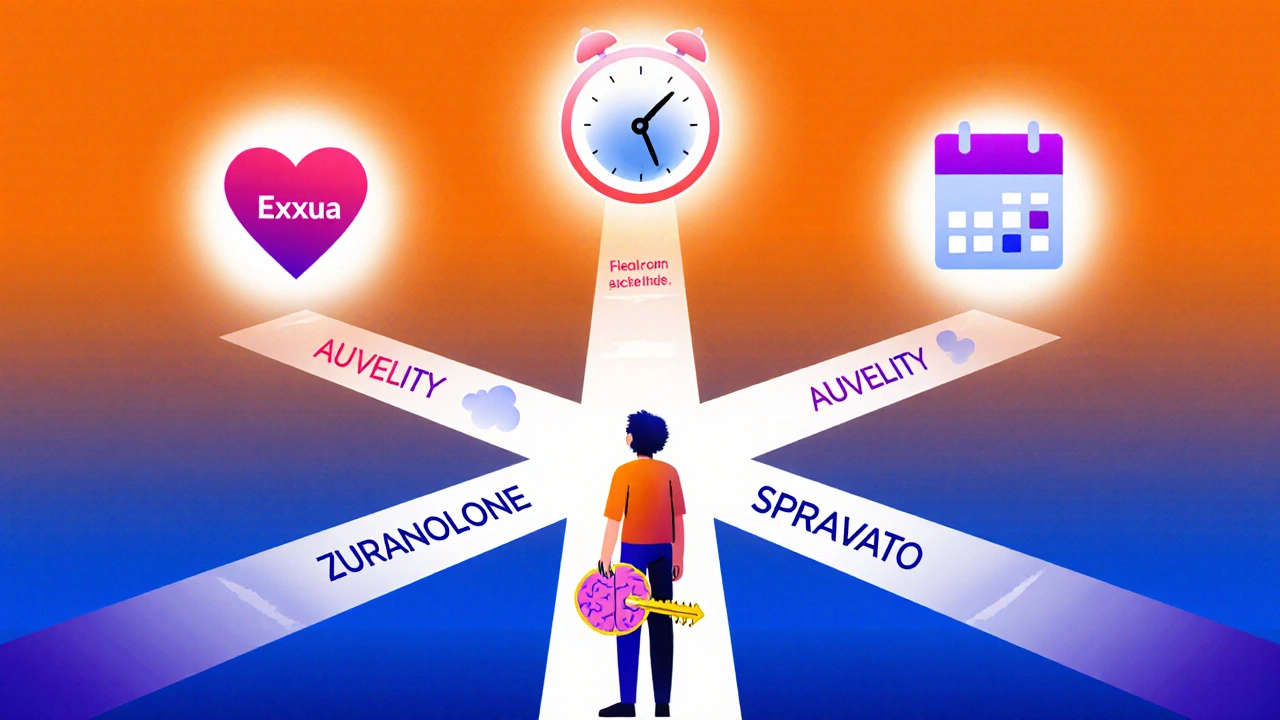
New antidepressants like Exxua, Zuranolone, and SPRAVATO offer faster relief and fewer side effects than traditional SSRIs. Learn how they work, who they help most, and what to expect in 2025.
New Antidepressants: What’s Changed and What Actually Works
When we talk about new antidepressants, modern medications designed to treat depression with improved safety and targeting over older drugs. Also known as next-generation antidepressants, they’re not just updated versions—they’re built differently, aiming for faster relief and fewer side effects. The old standbys like fluoxetine or sertraline still work for many, but if you’ve tried them and didn’t get relief, or if the drowsiness, weight gain, or sexual side effects were too much, the newer options might be what you’ve been waiting for.
One big shift is in how these drugs target the brain. While older SSRIs, selective serotonin reuptake inhibitors that increase serotonin levels to lift mood. Also known as serotonin boosters, they focus mostly on serotonin, newer ones like vortioxetine and brexanolone work on multiple neurotransmitters at once—serotonin, norepinephrine, dopamine, even glutamate. That’s why some people feel better faster, sometimes in days instead of weeks. Another game-changer is esketamine, a nasal spray approved for treatment-resistant depression, a form of depression that doesn’t improve after trying at least two different antidepressants. Also known as TRD, it. It’s not a typical pill—it’s used under medical supervision and can bring rapid relief when nothing else does.
Side effects still matter. A lot of these new drugs promise less sexual dysfunction or weight gain, but they come with their own risks. Esketamine can cause dizziness or dissociation. Brexanolone requires a 60-hour hospital infusion. Some newer pills still cause nausea or headaches early on. What’s different now is that doctors have more tools to match the drug to the person—not just based on diagnosis, but on symptoms like fatigue, brain fog, or anxiety. If you’re tired all the time, a drug that boosts energy might be better than one that just calms you down. If you’re stuck in rumination, something that targets glutamate could help break the cycle.
There’s also more focus on personalization. Genetic tests, symptom profiles, and even wearable data are starting to guide choices. You’re not just choosing between Prozac and Zoloft anymore—you’re choosing from a smarter, more varied toolkit. And while these new options can be expensive or hard to access, the trend is clear: the goal isn’t just to reduce symptoms, but to restore function. To help people sleep better, focus at work, reconnect with family—not just feel a little less sad.
Below, you’ll find real comparisons and practical insights on what these new options actually look like in everyday use. From cost and access to how they stack up against older meds, you’ll see what’s working for real people—and what’s still a gamble.