Alfacalcidol vs Calcitriol: Which Vitamin D Analog Is Best?
When doctors talk about vitamin D therapy, the names alfacalcidol and calcitriol often pop up. Both are synthetic forms of the hormone that regulates calcium, but they aren’t interchangeable. This guide breaks down how each works, who should use which, and what side‑effects to watch for.
What are Vitamin D Analogs?
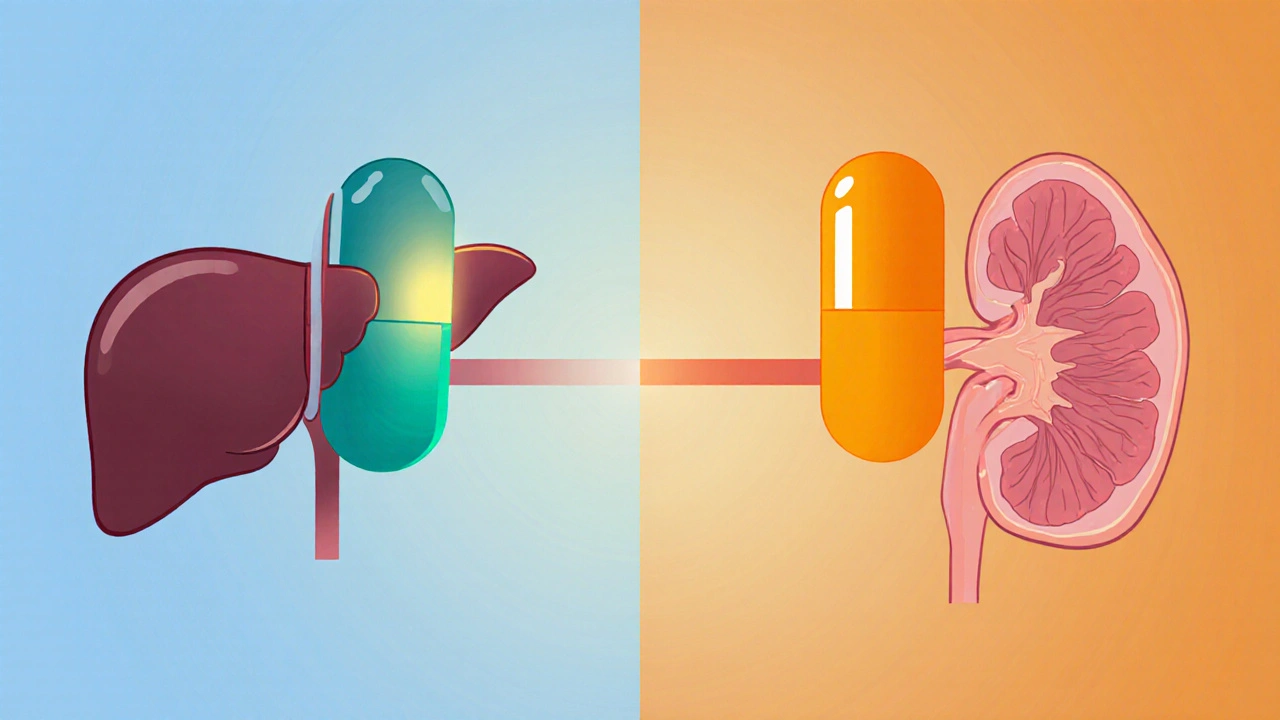
Vitamin D isn’t a single molecule; it’s a family of related compounds that travel through the liver and kidney before becoming the active hormone that tells the gut to absorb calcium. Synthetic versions-called Vitamin D analog is a chemically modified form of the natural hormone designed to mimic its actions in the body-let clinicians fine‑tune treatment for people whose kidneys can’t finish the conversion process.
Alfacalcidol: How It Works and Who Needs It
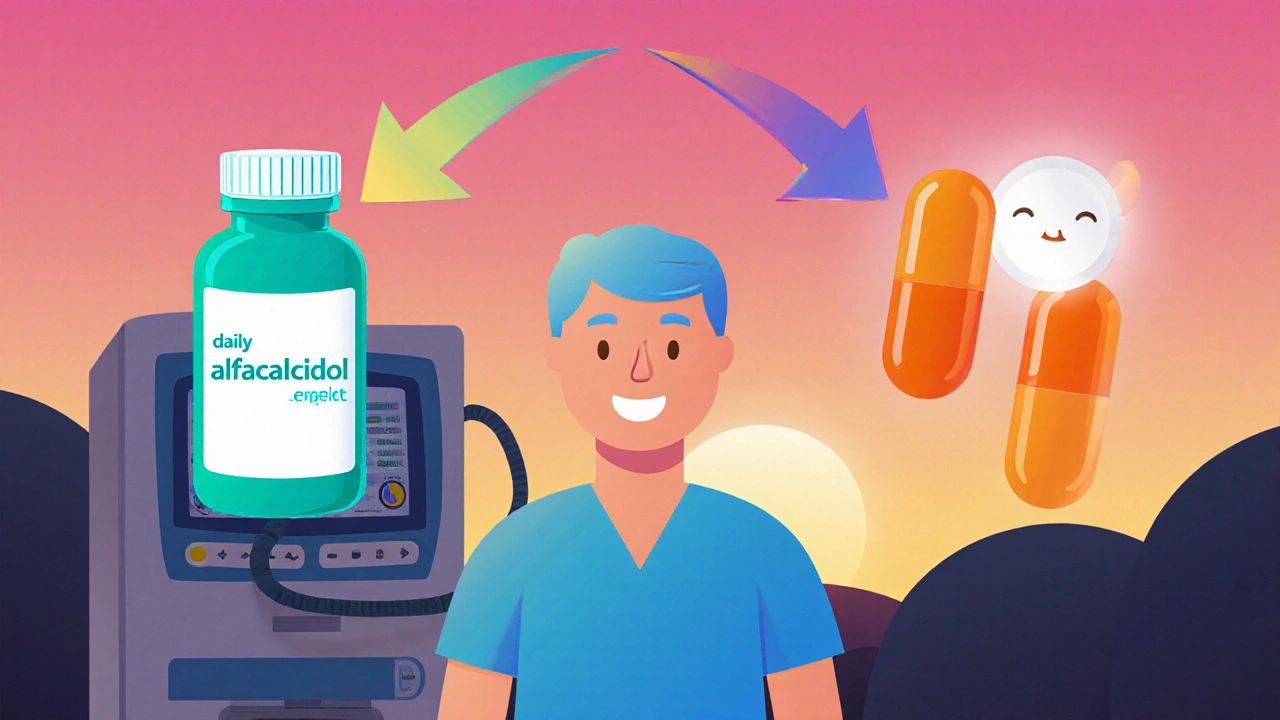
Alfacalcidol is a pro‑drug that requires only one activation step in the liver to become calcitriol, the body’s most potent form of vitamin D. Because it skips the kidney step, it’s a go‑to option for patients with chronic kidney disease (CKD) who can’t convert regular vitamin D efficiently.
- Key activation: Liver 25‑hydroxylation → active calcitriol
- Typical uses: CKD‑related secondary hyperparathyroidism, hypocalcemia, osteomalacia, and certain cases of osteoporosis
- Common dose: 0.5-2 µg daily, adjusted based on serum calcium and phosphate levels
- Side‑effects to monitor: Hypercalcemia, hyperphosphatemia, and occasional nausea
Because alfacalcidol bypasses the kidney, clinicians can start low and titrate up while checking labs every 1-2 weeks during the initiation phase.
Calcitriol: The Fully Active Form
Calcitriol is the 1,25‑dihydroxyvitamin D3 molecule that the kidneys normally produce. It’s already in its most potent state, so no further conversion is needed.
- Key activation: None-administered as the active hormone
- Typical uses: Hypocalcemia due to hypoparathyroidism, renal osteodystrophy, and severe vitamin D deficiency when rapid correction is required
- Common dose: 0.25-0.5 µg daily; some protocols use 0.25 µg three times weekly for maintenance
- Side‑effects to monitor: Same as alfacalcidol-primarily hypercalcemia, but because it’s already active, the therapeutic window is narrower
Calcitriol is ideal when the patient’s kidneys are still able to regulate calcium and phosphate, or when a rapid rise in active vitamin D is clinically necessary.
Head‑to‑Head Comparison
| Aspect | Alfacalcidol | Calcitriol |
|---|---|---|
| Activation requirement | One liver hydroxylation | Already active |
| Primary clinical use | CKD‑related secondary hyperparathyroidism | Hypoparathyroidism, rapid correction of deficiency |
| Typical starting dose | 0.5 µg - 2 µg daily | 0.25 µg - 0.5 µg daily |
| Monitoring focus | Serum calcium, phosphate, PTH | Serum calcium, especially after dose changes |
| Risk of hypercalcemia | Moderate - titratable | Higher - narrower therapeutic window |
| Cost (UK 2025) | £0.30 per 0.5 µg tablet | £0.45 per 0.25 µg capsule |
How to Choose the Right Analog
Deciding between alfacalcidol and calcitriol isn’t a matter of “which is cheaper” alone. Consider these factors:
- Kidney function: If eGFR is below 30 mL/min/1.73 m², alfacalcidol usually wins because the kidney can’t finish the activation process.
- Calcium baseline: Patients already flirting with high calcium levels may need calcitriol’s tighter dosing schedule, but they also need close lab checks.
- Desired speed of correction: For acute hypocalcemia, calcitriol’s immediate activity can bring levels up faster.
- Convenience: Alfacalcidol’s once‑daily dosing fits most chronic regimens, while calcitriol sometimes uses thrice‑weekly schedules.
- Drug interactions: Both interact with thiazide diuretics and calcium‑based antacids, but calcitriol’s effect is more pronounced.
In practice, many endocrinologists start patients on alfacalcidol for CKD‑related bone disease, then switch to calcitriol if a rapid rise in calcium is needed during a surgical recovery.
Practical Tips for Patients and Clinicians
- Always check serum calcium, phosphate, and PTH before adjusting the dose.
- Educate patients to report symptoms like nausea, muscle weakness, or excessive thirst-early signs of hypercalcemia.
- For patients on dialysis, consider weekly vitamin D analog dosing (e.g., alfacalcidol 1 µg three times per week) to match treatment sessions.
- Remember that dietary calcium intake influences dosing. A high‑calcium diet may require a lower analog dose.
- Review concomitant medications. Loop diuretics increase calcium excretion, which may mask rising serum calcium.
Frequently Asked Questions
Is alfacalcidol safe for patients without kidney disease?
Yes, but it’s usually reserved for kidney patients because they benefit most from the liver‑only activation step. In healthy kidneys, calcitriol often provides tighter control.
Can I take both alfacalcidol and calcitriol together?
Combining them raises the risk of severe hypercalcemia and is generally discouraged unless a specialist explicitly orders a split regimen for a very specific clinical scenario.
How quickly does calcitriol raise blood calcium?
Calcitriol can increase serum calcium within 24‑48 hours, making it useful for acute hypocalcemia after surgery or trauma.
What lab values signal I need to adjust my dose?
Target calcium: 2.2-2.6 mmol/L; phosphate: 0.8-1.5 mmol/L; PTH: aim for the middle of the reference range. Any sustained drift outside these windows warrants a dose tweak.
Are there dietary restrictions while on these analogs?
No strict bans, but patients should avoid excessive calcium supplements unless prescribed, and keep vitamin D‑rich foods (like fortified milk) in moderation.
Choosing the right vitamin D analog hinges on kidney function, how fast you need to raise calcium, and the patient’s overall mineral balance. By matching the drug’s activation pathway to the individual’s physiology, clinicians can avoid complications and keep bones strong.

Michelle Capes
Thx for the clear breakdwn, really helpful! 😊
Dahmir Dennis
When I first encountered the hype surrounding vitamin D analogs, I was convinced that every new compound was a miracle waiting to be marketed.
The pharmaceutical industry loves to dress up a simple calcium regulator in a veil of scientific mystique.
Alfacalcidol, a pro‑drug, is praised as if it were a revelation, yet its only advantage is a single hepatic hydroxylation step.
Likewise, calcitriol is lauded for being the fully active molecule, but that makes it a double‑edged sword in the hands of an inattentive prescriber.
The notion that clinicians can simply swap one for the other without considering the underlying renal physiology is dangerously naive.
One must remember that the kidney’s role in activating vitamin D is not a trivial footnote.
Ignoring this fact is tantamount to prescribing fireworks to a fireworks‑phobic audience.
Moreover, the dosing tables presented in the guide, while tidy, obscure the real‑world variability in patient absorption and compliance.
Patients on dialysis often have erratic dietary calcium intake, which can swing serum calcium levels dramatically.
The guide’s suggestion to titrate alfacalcidol every one to two weeks assumes perfect lab turnaround, a luxury most clinics do not have.
Meanwhile, the claim that calcitriol’s therapeutic window is narrower borders on alarmist hyperbole, ignoring that careful monitoring can mitigate most risks.
The economic argument, citing a few pennies per tablet, belittles the true cost of hypercalcemia complications.
Hypercalcemia can lead to nephrocalcinosis, cardiac arrhythmias, and even irreversible bone pain, none of which are cheap to treat.
It would be far more responsible to emphasize patient education over simplistic cost comparisons.
In short, the guide’s brilliance is dimmed by its occasional cavalier attitude toward patient safety.
Marilyn Pientka
Your reductive sarcasm overlooks the nuanced pharmacodynamics that dictate analog selection; renal 1α‑hydroxylase activity, calcium‑sensing receptor modulation, and PTH feedback loops are not mere footnotes. The interdisciplinary consensus among endocrinologists and nephrologists emphasizes that alfacalcidol’s hepatic activation circumvents the variable renal enzymatic capacity, thereby offering a more predictable serum 1,25‑(OH)₂D profile. By contrast, calcitriol’s immediate bioavailability mandates vigilant monitoring of ionized calcium and phosphate to preempt iatrogenic hyperphosphatemia. Disregarding these mechanistic distinctions reduces complex therapeutic strategies to a binary cost‑analysis, which is intellectually dishonest. Furthermore, the claim that dosing intervals are impractical fails to account for integrated care pathways that synchronize lab draws with dialysis sessions, optimizing both safety and resource allocation. Acknowledging the heterogeneity of patient phenotypes is essential; a one‑size‑fits‑all approach is clinically untenable. Your argument would benefit from a deeper engagement with the primary literature rather than a superficial appraisal of pricing tables.
Jordan Levine
Wow, reading this feels like watching a drama unfold where the *real* heroes-our doctors-are battling the evil forces of bureaucracy! 😤💥 Alfacalcidol is the unsung champion for our kidney patients, stepping in where others fail. And calcitriol? It's the flashy but volatile sidekick that can blow up if mishandled. This guide finally gives a voice to the struggle we face in our hospitals every day. 🩺⚡️ Let’s make sure the right analog gets the spotlight it deserves, because patient lives are on the line, not just some spreadsheet!
Ekeh Lynda
the data presented in the guide is thorough but the narrative overemphasizes drama at the expense of objective analysis patients with chronic kidney disease benefit from alfacalcidol due to its reliance on hepatic conversion which bypasses impaired renal activation pathways the pharmacokinetic profile of alfacalcidol yields more stable serum levels reducing the frequency of hypercalcemic episodes however calcitriol remains indispensable in acute settings where rapid correction of hypocalcemia is required the guide correctly notes dose ranges but fails to address the variability introduced by concomitant medications such as thiazides and calcium supplements clinicians must tailor therapy to individual biochemical indices and not rely solely on generic dosing protocols the economic considerations are secondary to patient safety especially when the cost of managing complications far exceeds the marginal price difference between the analogs careful monitoring of calcium phosphate product remains the cornerstone of therapy
Mary Mundane
Both analogs have their place, but the guide could have highlighted the importance of individualized dosing more clearly.
Amanda Vallery
Just a quick note the typical starting dose for alfacalcidol is usually 0.25‑0.5 µg daily not 0.5‑2 µg as stated.
Lindy Hadebe
Well, that's a minor detail but still worth mentioning.