Hyponatremia and hypernatremia are common, dangerous electrolyte disorders in kidney disease. Learn how CKD disrupts sodium balance, the real risks, and how to manage them safely without worsening kidney function.
Kidney Disease: Causes, Risks, and Management
When dealing with Kidney disease, a condition where the kidneys lose filtering ability over time. Also known as renal disease, it can start slowly and become serious if ignored. The same page often mentions Chronic kidney disease, the long‑term stage of kidney damage, which may lead to Dialysis, a medical process that takes over the kidneys' filtering work when function falls below a critical threshold.
One of the biggest drivers behind kidney disease is Hypertension, high blood pressure that strains the delicate vessels inside the kidneys. When pressure stays elevated, tiny blood vessels get damaged, reducing filtration efficiency and pushing the disease toward chronic stages. Another major contributor is Diabetes, high blood sugar that harms kidney tissue through advanced glycation end‑products. Together, these two conditions form a potent combo: hypertension accelerates diabetic kidney injury, and diabetes makes blood pressure harder to control.
Key Factors and Treatment Options
Understanding kidney disease means looking at three linked parts: the underlying cause, the functional decline, and the therapeutic response. First, lifestyle factors such as excess salt, weight gain, and smoking add stress to the kidneys. Second, lab markers like estimated glomerular filtration rate (eGFR) and albumin‑to‑creatinine ratio give a clear picture of how fast the disease is progressing. Finally, treatment options range from medication adjustments to invasive procedures. For many patients, controlling blood pressure with ACE inhibitors or ARBs can slow the drop in eGFR, while tight glucose control cuts down on diabetic damage.
When medication alone isn’t enough, doctors turn to renal replacement therapies. Dialysis comes in two flavors—hemodialysis at a center or peritoneal dialysis at home—each designed to clear waste and balance electrolytes. In cases where kidney function falls below roughly 10‑15% of normal, transplantation becomes the preferred long‑term solution. Transplants require careful immunosuppressive regimens, but they often restore quality of life far beyond what dialysis can offer.
Preventive care is the most cost‑effective strategy. Routine screening for protein in the urine, especially in people with diabetes or hypertension, catches early damage before symptoms appear. Dietary tweaks—lowering sodium, limiting animal protein, and staying hydrated—help preserve the remaining nephrons. Physical activity improves cardiovascular health, which indirectly protects kidney vessels.
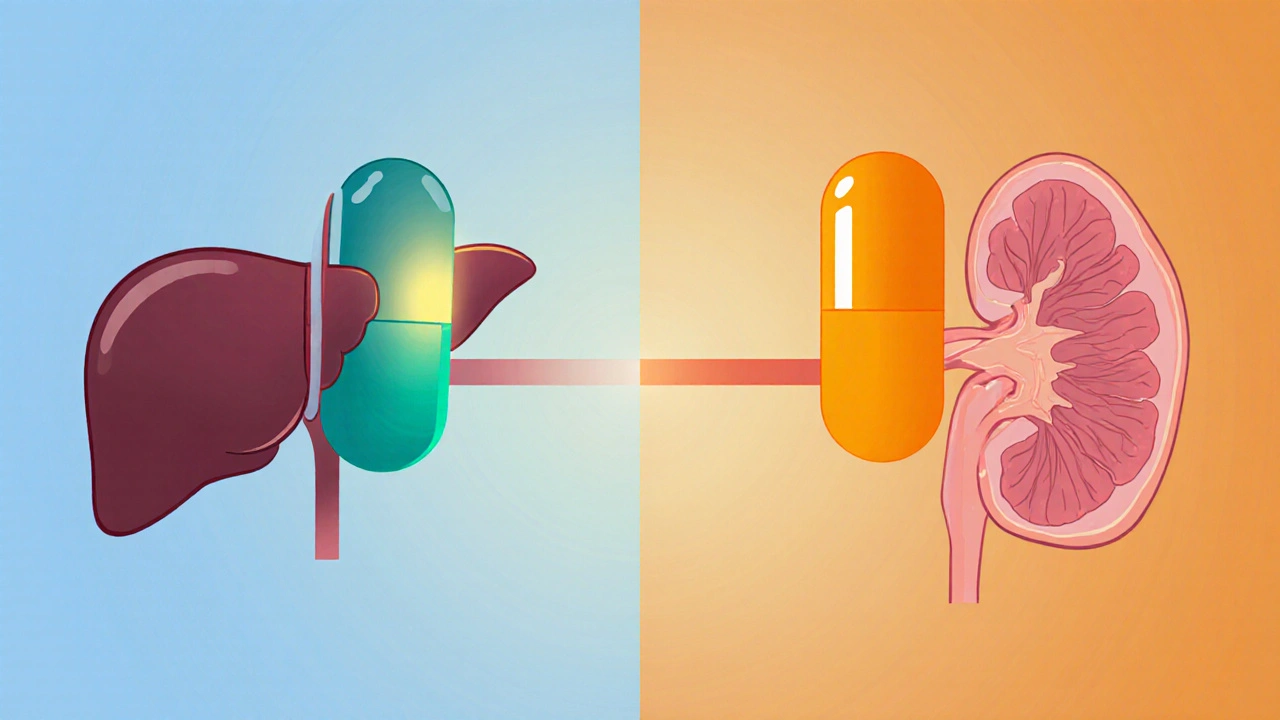
Patients also need to watch their medication list. Some drugs, like NSAIDs or certain antibiotics, can reduce renal blood flow and worsen kidney function. A pharmacist’s review can spot these hidden risks and suggest safer alternatives. Education about proper dosing, especially for over‑the‑counter meds, is a key step in avoiding accidental injury.
Healthcare teams play a central role in coordinating care. Nephrologists, dietitians, and social workers collaborate to create individualized plans that address medical, nutritional, and psychosocial needs. This multidisciplinary approach improves adherence to treatment and reduces hospital readmissions.
Because kidney disease often coexists with heart disease, cardiovascular risk management is inseparable from renal care. Controlling lipid levels, smoking cessation, and regular aerobic exercise lower the chance of heart attacks that can further harm kidney perfusion.
Technology is also reshaping kidney disease management. Portable creatinine monitors and telehealth visits let patients track their labs from home, while electronic alerts in clinic software flag dangerous medication combinations before they’re prescribed.
Looking ahead, researchers are testing new drugs that target fibrosis pathways—one promising class aims to block the protein TGF‑β, which drives scar formation in the kidneys. Early trials show slower eGFR decline, hinting at a future where we can halt the disease rather than just manage its symptoms.
All of these topics intersect in the articles you’ll find below. Whether you’re curious about how blood pressure meds affect kidney health, want a step‑by‑step guide to dialysis options, or need practical tips for medication safety, the collection offers clear, actionable information that builds on the basics covered here.
Continue scrolling to explore detailed guides, comparisons, and expert advice that will help you navigate kidney disease with confidence.
Compare alfacalcidol and calcitriol, learn how each works, best uses, dosing, side‑effects and how to pick the right vitamin D analog for kidney or bone health.