Learn which opioids are safe for kidney failure, how to adjust doses by GFR, and practical tips for monitoring side effects.
Fentanyl, Buprenorphine, and Kidney Health: What You Need to Know
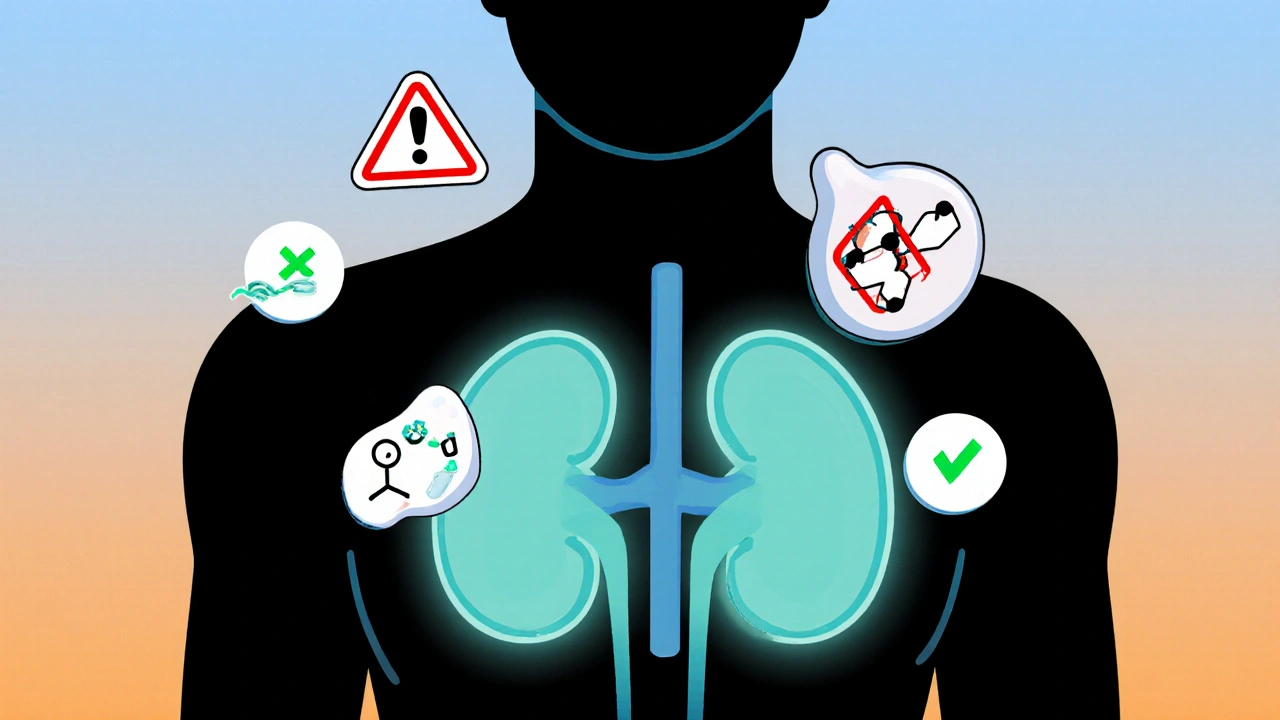
When you’re managing chronic pain with medications like fentanyl, a powerful synthetic opioid used for severe pain, often in cancer or post-surgery settings or buprenorphine, a partial opioid agonist commonly used for pain relief and opioid use disorder treatment, your kidneys might be working harder than you realize. These drugs don’t just affect your brain—they’re processed, filtered, and cleared by your renal system, the network of organs including kidneys, ureters, and bladder responsible for filtering blood and removing waste. If your kidneys aren’t functioning well, even standard doses can build up and cause dangerous side effects.
People with kidney disease, especially those on dialysis or with reduced glomerular filtration rate (GFR), need special care. Fentanyl is mostly broken down by the liver, but its metabolites can stick around longer if kidneys aren’t clearing them. That means drowsiness, slowed breathing, or confusion could sneak up on you—even if you’ve taken the same dose for months. Buprenorphine is a bit kinder to kidneys; it’s mainly cleared by the liver and excreted in bile. But its metabolite, norbuprenorphine, still relies on kidney function. Studies show that patients with severe kidney impairment may need lower doses or longer gaps between doses to avoid buildup. It’s not just about the drug itself—it’s about how your body handles it over time.
What does this mean for you? If you’re taking either medication and have been told you have kidney problems, don’t assume your current dose is safe. Talk to your doctor about checking your kidney function with a simple blood test—creatinine and eGFR levels tell the real story. Watch for signs like swelling in your ankles, fatigue, or changes in urination. These aren’t always obvious until it’s too late. Many people don’t realize their kidneys are struggling until they start feeling worse overall. That’s why monitoring isn’t optional—it’s part of staying safe.
There’s also the matter of drug interactions. If you’re on other meds—like NSAIDs for arthritis, diuretics for fluid retention, or even some antibiotics—your kidneys are under more stress. Combine that with fentanyl or buprenorphine, and the risk goes up. You don’t need to stop your pain treatment, but you do need a plan that accounts for your kidney health. That plan should be personal. What works for someone else might not work for you.
Below, you’ll find real-world guides that dig into how these drugs interact with other treatments, what to watch for, and how to make smarter choices if you’re managing pain while dealing with kidney issues. These aren’t theoretical articles—they’re written for people who need to live with these medications, not just read about them.