Chemotherapy: How Cytotoxic Drugs Work and What Side Effects to Expect
Chemotherapy isn't a single drug. It’s a whole system of powerful chemicals designed to kill cancer cells by attacking anything that divides quickly. That’s the core idea: cancer cells multiply nonstop, and chemo drugs exploit that weakness. But here’s the catch - so do your hair follicles, your gut lining, and your bone marrow. That’s why side effects happen. And while it sounds brutal, chemotherapy has saved millions of lives since the first trial in 1942, when a nitrogen mustard compound was used on a patient with lymphoma at Yale. Today, over 100 different cytotoxic drugs are in use, each with its own way of breaking down cancer cells.
How Chemotherapy Targets Cancer Cells
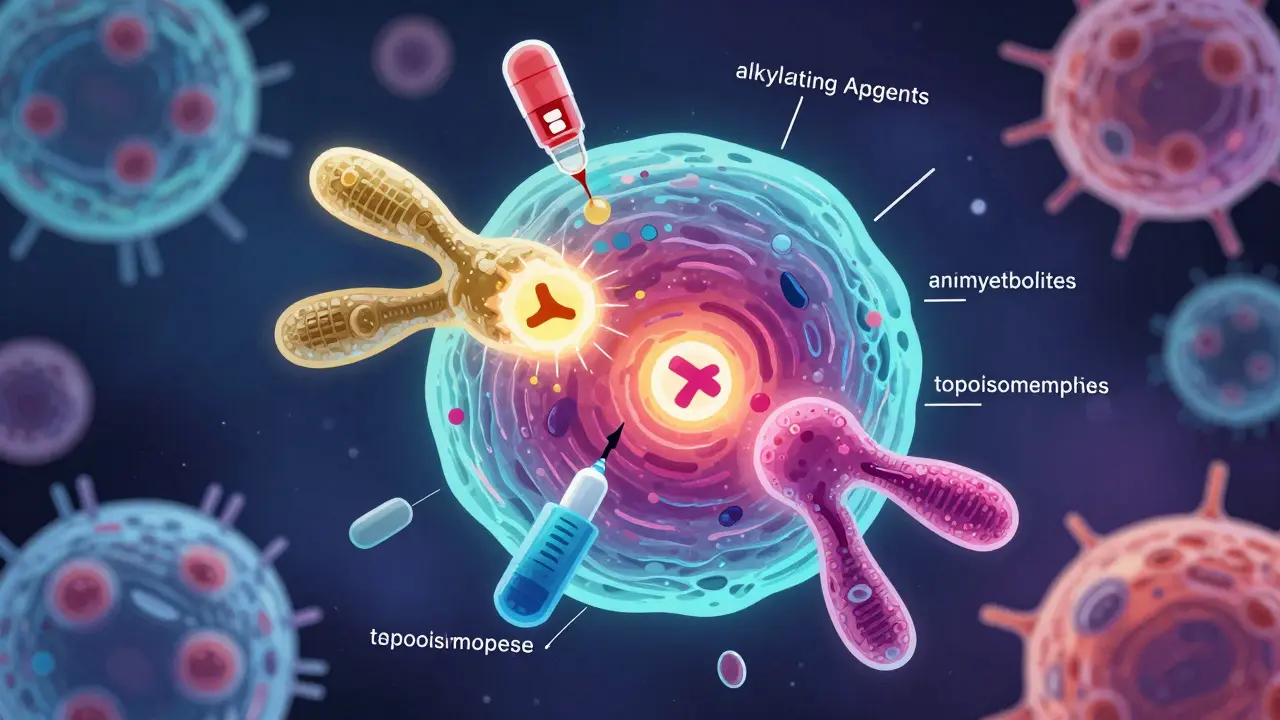
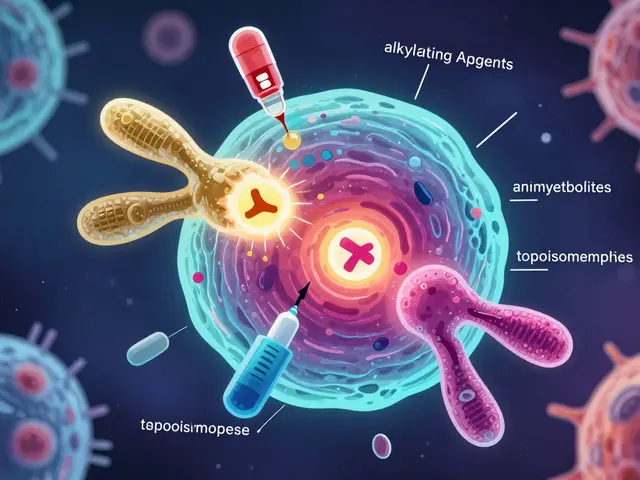
Chemotherapy drugs don’t just randomly poison cells. They’re engineered to interfere with specific parts of the cell division process. There are six main classes, and each works differently. Alkylating agents like cyclophosphamide stick chemical groups onto DNA, making it impossible for the cell to copy its genetic code. Without that, the cell can’t divide - it just dies. Antimetabolites like 5-fluorouracil are imposters. They look like the building blocks cells need to make DNA and RNA, but once they’re inside, they jam the machinery. The cell tries to use them, and it collapses.
Anthracyclines, such as doxorubicin, slip between DNA strands and block an enzyme called topoisomerase II. That enzyme normally untangles DNA during replication. When it’s stuck, the DNA breaks. Plant alkaloids like vincristine and paclitaxel attack the cell’s skeleton. Microtubules are like tiny train tracks that pull chromosomes apart during division. Vincristine stops them from forming. Paclitaxel does the opposite - it freezes them in place. Either way, the cell can’t split. Topoisomerase inhibitors like etoposide do something similar, but they target a different enzyme. The result? DNA damage that cancer cells can’t repair.
These drugs are given in cycles - usually every 2 to 6 weeks. That’s not just tradition. It’s science. Healthy cells need time to recover between doses. Cancer cells, which are often more damaged and less organized, recover slower. This gives your body a fighting chance. About 65% of chemotherapy is delivered through IV infusion. The rest comes as pills, injections into the spinal fluid, or directly into the abdomen or artery, depending on where the cancer is.
Why Chemotherapy Still Matters in 2026
You might hear that targeted therapies and immunotherapies are replacing chemo. That’s partly true - but only for certain cancers. For many, chemo is still the first line of defense. In acute myeloid leukemia, 78% of patients still start with chemotherapy. In ovarian cancer, it’s used in 95% of cases. In colorectal cancer, it’s in 85%. Even in breast cancer, where targeted drugs like Herceptin are common for HER2-positive cases, chemo is still given to nearly 70% of patients, often before surgery to shrink tumors.
Why? Because chemo works fast and broadly. It doesn’t need a specific genetic marker to attack. If a tumor has mixed cell types - and most do - chemo can hit them all. It also crosses the blood-brain barrier, something many newer drugs can’t do. That’s why it’s still used for brain metastases. And while targeted drugs might work better for a subset of patients, chemo works for a lot more. A 2021 trial showed that patients with breast cancer who got chemo before surgery had a 40-60% chance of having no detectable cancer left at removal. Those patients lived longer.
Even in cancers where targeted drugs are preferred, chemo often plays a supporting role. For example, in lung cancer with EGFR mutations, patients start with a targeted pill. But when the cancer resists, chemo comes back in. The same is true for many other cancers. Chemo isn’t the future - but it’s still the backbone.
Common Side Effects and How They’re Managed Today
Side effects haven’t disappeared - but they’ve gotten far more manageable. In the 1990s, severe nausea hit 70-80% of patients on strong chemo regimens. Today, thanks to drugs like ondansetron and aprepitant, that number is down to 10-20%. That’s a massive win. Still, other side effects remain common.
Fatigue is the most reported issue - mentioned by 82% of patients in online forums. It’s not just being tired. It’s bone-deep exhaustion that sleep doesn’t fix. Studies show 30 minutes of moderate exercise daily - like walking or light cycling - reduces fatigue by 25-30%. That’s backed by 17 clinical trials. Hydration helps too. Drinking 1-2 liters of water a day can ease mild fatigue and prevent dehydration from nausea or diarrhea.
Hair loss affects 78% of patients. Scalp cooling caps have changed the game. In breast cancer patients on taxane-based chemo, these caps reduce hair loss from 65% to just 25%. That’s a huge improvement. But it’s not perfect. Some people still lose hair, and the cold can be uncomfortable. Still, many say it gives them back a sense of control.
Chemotherapy brain - or chemo brain - is real. About 75% of patients report trouble focusing, remembering names, or finding words during treatment. Three in ten still have issues six months after finishing. Meditation helps. A 2021 study in JAMA Oncology found that patients using apps like Calm or Headspace for 20 minutes a day saw a 30-40% reduction in cognitive complaints. It’s not a cure, but it’s a tool.
Peripheral neuropathy - tingling, numbness, or pain in hands and feet - happens in 30-40% of people on drugs like paclitaxel or carboplatin. Five to ten percent have lasting damage. The key is early reporting. If you feel numbness, tell your doctor right away. Avoid cold surfaces, wear gloves when handling things, and don’t wait to see if it gets worse.
What Patients Actually Say About Chemotherapy
Real people, real experiences. On Reddit’s r/cancer, 1,247 posts from 2023 showed that fatigue, hair loss, and nausea were the top three complaints. But many also said the same things: “I didn’t realize how much better nausea control is now,” and “My care team made all the difference.”
One woman wrote: “I could handle the vomiting. But the brain fog made me feel like I was losing myself. I couldn’t focus at work. I forgot my daughter’s favorite song.” That’s chemo brain. Another said: “Imodium helped my diarrhea. Nothing helped the metallic taste in my mouth.” That’s a lesser-known side effect - altered taste - and it’s surprisingly common.
Some side effects are hidden. Dexamethasone, a steroid often given before chemo to prevent nausea, causes insomnia in 43% of patients. That’s not just a nuisance - it worsens fatigue and brain fog. Sleep hygiene matters. Avoid screens at night. Keep your room cool. Talk to your doctor about alternatives if it’s wrecking your rest.
What patients praise most? Support systems. Nurses who check in. Nutritionists who suggest bland foods like toast and bananas. Social workers who help with transportation. Chemo isn’t just drugs. It’s a whole team.
What You Need to Know Before Starting
If you’re about to begin chemo, here’s what matters most. First, know your regimen. Ask: What drug am I getting? How often? How long will each session take? Is it IV or oral? Knowing this helps you plan your life.
Second, know the warning signs. A fever of 100.4°F or higher during chemo is an emergency. It could mean your white blood cell count has dropped too low - a condition called neutropenic fever. Call your oncology team immediately. Don’t wait. Don’t go to the ER without calling first - they’ll want to know what chemo you’re on.
Third, track your symptoms. Keep a simple journal. What time did you feel tired? Did you eat? Did you have diarrhea? Did your hands tingle? This helps your team adjust your care. One study found that 85% of patients mastered basic symptom management by their third cycle. You’re learning, not failing.
Fourth, don’t assume supplements help. Some patients take vitamin D hoping to reduce nerve damage from Taxol. But the American Society of Clinical Oncology says there’s not enough proof to recommend it. On the other hand, medical cannabis is gaining attention. A 2023 study showed CBD and THC blends reduced neuropathic pain by 55% in some patients. Talk to your doctor before trying anything.
What’s New in Chemotherapy Care
Chemo isn’t standing still. In June 2023, the FDA approved trilaciclib (Cosela) - the first drug designed to protect bone marrow during chemo. It’s used for small cell lung cancer patients and helps keep white blood cells and red blood cells from crashing. That means fewer infections, fewer transfusions, and fewer delays in treatment.
Scalp cooling is now in the National Comprehensive Cancer Network’s 2024 guidelines. It’s not a magic trick, but for many, it’s a game-changer. And research into how chemo affects the brain is accelerating. Mindfulness, sleep, and movement aren’t just nice ideas - they’re part of modern cancer care.
Even as new therapies rise, chemotherapy remains essential. For cancers without known targets - like many types of ovarian, pancreatic, and triple-negative breast cancer - chemo is still the most effective tool. The goal now isn’t to replace it. It’s to make it smarter, gentler, and more personal. That’s what’s happening now - one cycle, one side effect, one patient at a time.

Juan Reibelo
Chemotherapy is brutal, but it’s also one of the most precise forms of violence we’ve ever invented-targeting chaos with chaos. I’ve seen it work on my uncle’s lymphoma when nothing else would touch it. The side effects? Yeah, they’re awful. But I’d take fatigue and hair loss over a tombstone any day.
Karen Conlin
Let me tell you something-chemo isn’t just drugs. It’s a whole ecosystem of care. Nurses who remember your name, nutritionists who suggest bland toast because your tongue feels like sandpaper, social workers who drive you to appointments when you can’t stand up straight. This isn’t just science-it’s humanity in action. And if you think it’s outdated, you haven’t talked to a single patient who’s alive today because of it. Chemo’s the backbone because it doesn’t care if your tumor has a fancy mutation-it just kills the damn thing.
asa MNG
lol so chemo is just poison?? 😂 i mean like… why not just eat more kale?? 🥬💀 i heard turmeric cures everything. also my cousin’s dog got cancer and she gave it cbd treats and now he’s running around like a maniac. science is a cult. #chemoisfake #naturalhealing
Chloe Hadland
I just finished my third cycle. The brain fog is real. I forgot my mom’s birthday. I cried for an hour over a burnt toast. But I’m alive. And I’m learning. Slowly. One nap at a time.
Michael Camilleri
People treat chemo like it’s sacred. It’s not. It’s a blunt instrument. We’ve been using it since the 1940s because we’re lazy. We don’t want to wait for better science. We want quick fixes. And now we’re poisoning people for profit. The pharmaceutical industry loves chemo because it’s repeatable. It’s not healing-it’s a revenue stream wrapped in a white coat.
Darren Links
Yeah well in my country we don’t use this junk. We use ozone therapy and fasting. Chemo is a western scam. Your body heals itself if you stop feeding it sugar and trust the universe. You’re just brainwashed by Big Pharma. I’ve seen people recover from stage 4 with nothing but lemon water and positive vibes.
Helen Leite
They’re lying about the side effects. The real reason you get hair loss is because the government put tracking chips in the chemo drugs so they can monitor your thoughts. Also, the ‘scalp cooling caps’? Those are just heat sensors. They’re recording your brainwaves. Don’t trust the doctors. They’re working for the shadow government. 🤫👁️🗨️
Marlon Mentolaroc
Interesting breakdown. But you missed one thing-chemo’s real cost isn’t just physical. It’s the psychological toll on families. The silent guilt of surviving when someone else didn’t. The way your partner stares at you like you’re a ghost. The way your kid asks if you’ll still be here next Christmas. The drugs don’t fix that. And nobody talks about it.
Gina Beard
Chemo works because it’s cruel. And cruelty has a purpose.