Antidepressant Overdose: Recognizing Serotonin Syndrome Warning Signs Early

When you start an antidepressant, you’re not just managing mood-you’re changing how your brain handles serotonin. That’s a good thing, unless it goes too far. Too much serotonin doesn’t just make you feel weird-it can trigger serotonin syndrome, a dangerous, sometimes deadly reaction that develops in hours, not days. And most people don’t see it coming.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn’t an allergy. It’s not a side effect you can just ‘tough out.’ It’s a toxic overload of serotonin in your nervous system, usually caused by mixing medications-or taking too much of one. It happens when drugs that boost serotonin-like SSRIs (sertraline, fluoxetine), SNRIs (venlafaxine, duloxetine), MAOIs (phenelzine), certain painkillers (tramadol, fentanyl), migraine meds (sumatriptan), or even cough syrups with dextromethorphan-pile up in your system.
The body doesn’t know how to handle the flood. Your nerves fire nonstop. Muscles spasm. Your heart races. Your temperature climbs. And your mind gets foggy. This isn’t anxiety. It’s not the flu. It’s a medical emergency.
The First Red Flags: What You’ll Actually Feel
Most people think serotonin syndrome starts with confusion or panic. But the earliest, most reliable sign? Tremors. A shaking in your hands, legs, or whole body that feels like you’ve had too much coffee-except you haven’t. It’s not just nervous energy. It’s your muscles twitching uncontrollably.
Right after that, you might notice:
- Muscle jerks or sudden spasms, especially in your arms or legs
- Restlessness-you can’t sit still, even if you’re exhausted
- Sweating like you’re in a sauna, even in a cool room
- Nausea, vomiting, or diarrhea-gut symptoms show up fast
- Dilated pupils that look wide and unresponsive to light
These signs often hit within an hour of taking a new medication or increasing a dose. Sixty percent of cases show up within six hours. That’s faster than most people realize. If you just started a new antidepressant, added a painkiller, or switched meds in the last 24 hours and you’re feeling off-don’t wait.
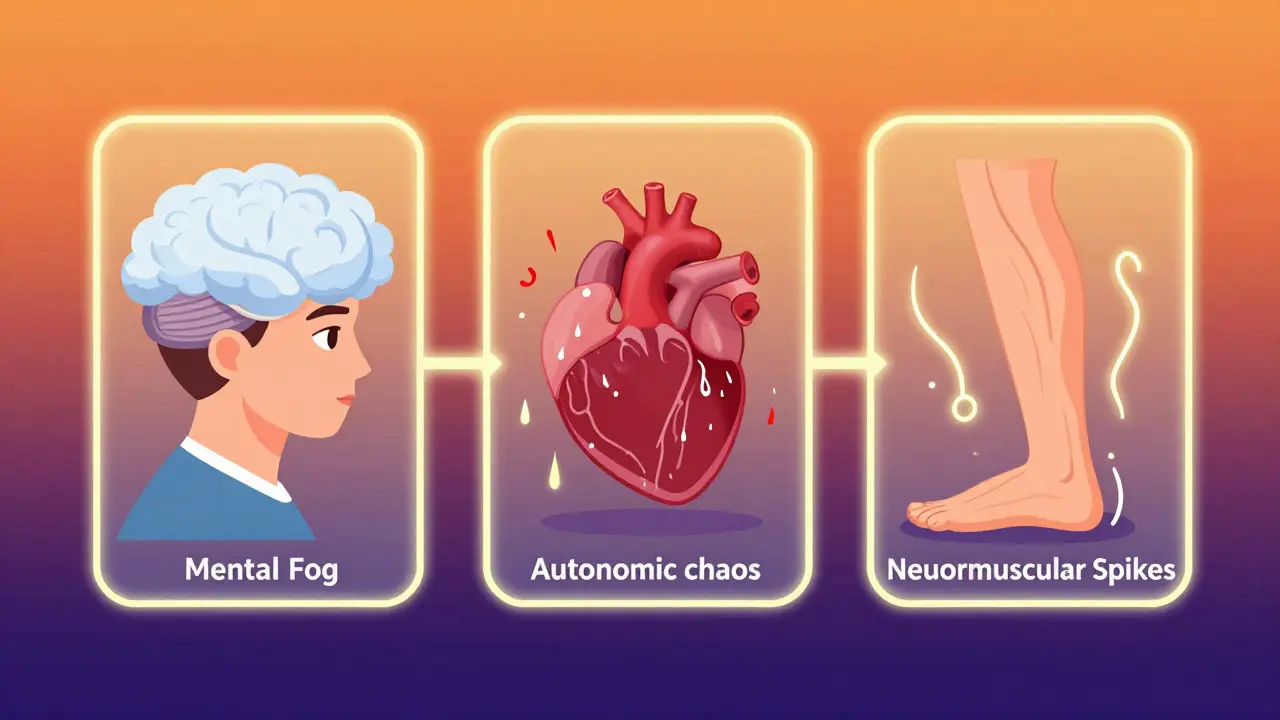
The Critical Triad: Mental, Autonomic, and Muscle Symptoms
Doctors use a simple framework to spot serotonin syndrome: mental changes, autonomic chaos, and neuromuscular chaos. If you see two of these, it’s likely.
Mental status changes: Confusion, agitation, hallucinations, or feeling like you’re losing touch with reality. In 78% of cases, people report mental fogginess. It’s not just being ‘stressed’-it’s a sudden shift in how you think.
Autonomic symptoms: Your body’s automatic systems go haywire. Heart rate over 100 bpm. Blood pressure spikes (systolic above 160). Body temperature climbs above 100.4°F. Breathing gets fast and shallow. You might sweat so much your clothes soak through.
Neuromuscular signs: This is where it gets serious. Clonus-a rhythmic, involuntary muscle contraction-is the hallmark sign. Try this: gently bend your foot upward. If your toes keep jerking up and down like a metronome, that’s clonus. It’s present in 92% of confirmed cases. You might also feel your muscles locking up (hypertonia), or your reflexes become crazy strong (hyperreflexia). A doctor can check this with a quick knee-tap test.
When It Turns Life-Threatening
Most cases are mild and improve quickly if caught early. But about 30% of people end up in the hospital. When it turns critical, you’ll see:
- Temperature above 101.3°F (38.5°C)
- Severe muscle rigidity-your limbs feel like concrete
- Seizures
- Irregular heartbeat or chest pain
- Loss of consciousness
At this point, your muscles are breaking down (rhabdomyolysis), your kidneys are under stress, and your organs start to fail. Death can happen from overheating above 106°F or from organ collapse. The mortality rate? Between 0.5% and 12%, depending on how fast you get help.
Why It’s So Often Missed
Doctors miss serotonin syndrome in about 25% of cases. Why? Because it looks like everything else.
It’s mistaken for:
- Neuroleptic malignant syndrome (NMS): Similar muscle rigidity, but slower to develop (days, not hours), and you’re lethargic, not agitated. Reflexes are weak, not overactive.
- Anticholinergic toxicity: Dry mouth, no sweating, constipation, urinary retention-opposite of serotonin syndrome’s sweating and diarrhea.
- Flu or anxiety: Fatigue, nausea, shakiness-common symptoms that get dismissed until it’s too late.
Reddit threads from people who’ve been through it are full of stories like: ‘I went to the ER with ‘flu symptoms’ and was sent home. Two hours later, I couldn’t stand up.’ Or: ‘My psychiatrist said it was just side effects. I ended up in ICU.’
How It’s Diagnosed-No Blood Test Needed
There’s no single blood test for serotonin syndrome. Serum serotonin levels don’t reliably predict symptoms. Instead, doctors use the Hunter Serotonin Toxicity Criteria, the gold standard. You need one of these:
- Spontaneous clonus
- Inducible clonus + agitation or sweating
- Ocular clonus + agitation or sweating
- Tremor + hyperreflexia
- Hypertonia + temperature above 100.4°F + ocular or inducible clonus
If you meet one of those, you have serotonin syndrome. That’s it. No labs. No scans. Just observation and history.

What to Do Right Now
If you suspect serotonin syndrome:
- Stop taking the medication(s) immediately. Don’t wait for a doctor’s call.
- Call 911 or go to the ER. This is not something to ‘wait and see.’
- Bring your pill bottles. Tell them exactly what you took, when, and how much.
- Don’t try to ‘cool down’ yourself. Don’t take cold showers or ice packs. Let medical staff manage your temperature safely.
In the hospital, treatment is straightforward:
- IV fluids to prevent dehydration
- Benzodiazepines (like lorazepam) to calm muscle spasms and agitation
- Cooling blankets or fans for high fever
- Cyproheptadine-an antidote given orally or through a tube-to block serotonin
Most people start improving within hours after treatment begins. Full recovery usually takes 24 to 72 hours if caught early.
How to Prevent It
Over 78% of cases happen when people take two or more serotonergic drugs together. Prevention is simple-but requires vigilance.
- Never combine antidepressants with other serotonin boosters without your doctor’s approval. That includes migraine meds, painkillers, herbal supplements (like St. John’s Wort), and even some OTC cough syrups.
- If switching from an MAOI to an SSRI, wait 14 days. This isn’t optional. It’s a hard FDA rule. Go shorter, and you risk overdose.
- Ask your doctor or pharmacist every time a new drug is added: ‘Could this interact with my antidepressant?’
- Keep a written list of every medication you take-including vitamins and supplements-and update it every time something changes.
Studies show that when patients get clear education about interactions, their risk drops by nearly half. And when doctors do full medication reviews, risk falls by 62%.
Final Reality Check
Serotonin syndrome is rising. Emergency visits jumped 22% year-over-year through mid-2024. More people are on antidepressants. More are taking multiple meds for pain, anxiety, migraines, or sleep. Polypharmacy is the new normal.
But here’s the truth: You don’t need to be afraid of your medication. You just need to be informed. If you’re on an SSRI or SNRI and you start feeling tremors, sweating, or mental confusion after a change in your meds-don’t ignore it. Don’t assume it’s ‘just anxiety.’ Don’t wait until you’re in pain. Act fast. Your life might depend on it.
Can serotonin syndrome happen with just one antidepressant?
Yes. While mixing medications is the most common cause, taking too high a dose of a single antidepressant-especially if you’re sensitive or have liver issues-can cause serotonin syndrome. It’s rare, but it happens.
How long does serotonin syndrome last?
If caught early and treated, symptoms usually start improving within hours and resolve fully in 24 to 72 hours. If it’s severe and treatment is delayed, symptoms can last longer, sometimes up to a week, especially if muscle breakdown or organ damage occurs.
Is serotonin syndrome the same as withdrawal?
No. Withdrawal happens when you stop a medication and your body reacts to its absence-symptoms like dizziness, irritability, or ‘brain zaps.’ Serotonin syndrome happens when there’s too much serotonin, usually after adding or increasing a drug. They’re opposites.
Can I check my serotonin levels at home?
No. There’s no reliable home test. Blood serotonin levels don’t correlate with symptoms, and the test isn’t used for diagnosis. Diagnosis is based on symptoms and medication history, not lab results.
Are some antidepressants riskier than others?
SSRIs cause about 62% of cases, SNRIs 24%, and MAOIs 8%. But the risk isn’t just about the drug-it’s about combinations. Even low-risk drugs become dangerous when mixed. MAOIs are the most dangerous if not used correctly, especially without the required 14-day washout period.
What should I tell my doctor if I think I have serotonin syndrome?
Be specific: ‘I started [medication] on [date] and now I have [tremors, sweating, confusion].’ List every pill, supplement, and OTC product you’ve taken in the last 72 hours. Mention if you’ve had clonus, muscle stiffness, or high temperature. Use the word ‘serotonin syndrome’-it helps them think of it faster.


Sue Stone
Just started sertraline last week and noticed my hands shaking a bit this morning. Thought it was caffeine, but now I’m freaking out a little. Thanks for this.
Stacy Thomes
THIS IS SO IMPORTANT. I almost died last year and no one believed me until I passed out. If you feel weird after a med change-GO TO THE ER. Don’t text your doctor. Don’t wait. Just go. Your life is worth more than your pride.
Oladeji Omobolaji
Back home in Nigeria, people mix antidepressants with herbal teas and traditional meds all the time. No one knows about this. I showed my cousin this post-he almost cried. We need more awareness here.
Janet King
Serotonin syndrome is underdiagnosed because symptoms mimic common conditions. Clinicians must always ask about medication combinations, especially when patients present with autonomic instability. Early recognition saves lives.
Vanessa Barber
Yeah but what if you just have anxiety? I’ve had tremors before and it wasn’t this. People are too quick to panic now. Maybe it’s not always serotonin syndrome.
Dawson Taylor
Clonus is the key. If you can’t reproduce it on exam, it’s not clonus. The Hunter Criteria are simple, reliable, and underused. This is why medical education needs to emphasize clinical signs over lab tests.
Anna Pryde-Smith
I went to the ER with ‘flu symptoms’ and they sent me home. I woke up 3 hours later with my legs locked and my heart pounding like a drum. They didn’t even ask about my meds. I was in ICU for 4 days. This isn’t hype. This is survival. If you’re on antidepressants, READ THIS. SAVE YOURSELF.
dana torgersen
...and yet... the brain... it’s not just serotonin... it’s the interplay... the delicate... balance... of neurotransmitters... you know?... and we’re just... tinkering... with chemicals... that evolved over millions of years... and now we’re mixing them like cocktails... and wondering why things go wrong...?... it’s... terrifying... really...
Sallie Jane Barnes
Thank you for writing this with such clarity. I’m a nurse and I’ve seen this too many times. Please, if you’re on meds-keep a list. Share it with every provider. Ask the question: ‘Could this interact?’ It’s not being difficult. It’s being smart.
Kerry Moore
Thank you for sharing your experience. This is precisely the kind of detailed, clinically accurate, and accessible information that saves lives. I’ve reviewed this with my patients and provided printed copies to their families. The Hunter Criteria should be taught in every primary care orientation. Your post is a public health asset.