A clear comparison of diacerein with NSAIDs, glucosamine, hyaluronic acid and other osteoarthritis treatments, covering mechanisms, efficacy, side‑effects and cost.
Osteoarthritis Treatment: What Works and Why
When dealing with Osteoarthritis Treatment, the range of medical, physical and lifestyle approaches used to relieve joint pain and improve function. Also known as OA therapy, it aims to keep you moving and limit disability. The first line of action often includes Physical Therapy, targeted exercises and manual techniques that strengthen muscles around the joint and Medication Management, the careful selection and monitoring of drugs like NSAIDs, corticosteroids, or analgesics. Together they form a core that many clinicians rely on when crafting a personalized plan. Strong osteoarthritis treatment plans also consider supplements, patient education, and, when needed, surgical options.
Physical therapy and patient education: the dynamic duo
Physical therapy isn’t just about stretching; it’s a science-backed method that improves joint stability, reduces pain, and restores range of motion. Studies show that patients who combine regular exercise with clear education about their condition see faster functional gains. Think of patient education as the bridge that translates complex medical advice into everyday actions—like knowing when to rest versus when to stay active. This relationship mirrors the findings from our article on chronic heart failure, where therapy outcomes sky‑rocket when patients understand their regimen. In osteoarthritis, the same principle applies: teaching proper movement patterns and pacing can prevent over‑use injuries and keep the joints healthier longer.
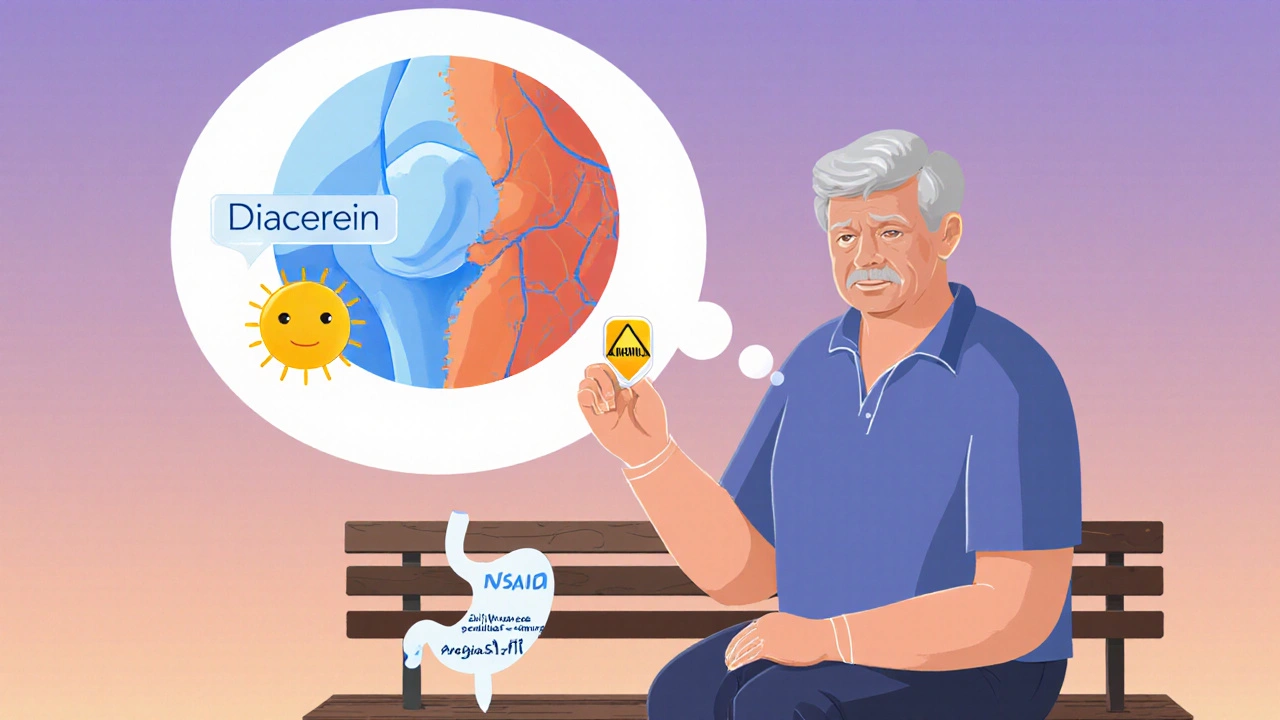
When it comes to medication, the goal is twofold: control inflammation and alleviate pain without causing side effects. NSAIDs are the workhorse, but they must be balanced against gastrointestinal risk, especially in older adults. That’s why many providers pair a low‑dose NSAID with a proton‑pump inhibitor, a strategy echoed in our guide on cheap generic Prilosec. For those who can’t tolerate NSAIDs, topical analgesics or intra‑articular injections become viable alternatives. Consistent medication adherence—something patient education directly supports—ensures steady symptom control and avoids flare‑ups that can set back progress.
Supplements like glucosamine, chondroitin, or omega‑3 fatty acids often enter the conversation. While evidence varies, some users report modest pain relief and improved joint lubrication. The key is to view supplements as a complement, not a replacement, for core therapies. In the same way that our article on hypercholesterolemia stresses early detection alongside lifestyle tweaks, osteoarthritis benefits from a combined approach: diet, weight management, and targeted nutrients work together to reduce joint load and inflammation.
For advanced disease, joint replacement becomes a realistic option. Joint Replacement, surgical substitution of damaged joint surfaces with artificial implants offers dramatic pain relief and functional restoration, especially when conservative measures have plateaued. The decision hinges on pain severity, functional limitation, and overall health. Our collection also touches on postoperative care and rehab—critical steps that echo the rehabilitation principles in our chronic heart failure piece.
All these pieces—exercise, medication, supplements, education, and surgery—interlock to form a comprehensive osteoarthritis management puzzle. Below, you’ll find articles that dive deeper into each component, from dosing tips for NSAIDs to the latest in physical therapy techniques. Whether you’re just starting to manage mild knee pain or preparing for a major surgical decision, the resources here will give you practical, evidence‑based guidance to move forward with confidence.