Calcitonin is a hormone that's been shown to have a positive impact on our bone health. It plays a crucial role in regulating bone mineral density, which is essential for maintaining strong bones. In addition, research has demonstrated that calcitonin can significantly reduce the risk of fractures in individuals with osteoporosis. This means that calcitonin therapies could be a vital tool in the fight against bone-related diseases, helping countless people maintain their mobility and independence. Overall, it's exciting to see how the effects of calcitonin could lead to improved bone health and a better quality of life for many.
Bone Mineral Density: What It Means and How to Improve It
Low bone mineral density raises fracture risk, and you might not notice it until a fall or a broken wrist. Bone mineral density (BMD) measures how dense your bones are and helps predict fracture risk. Knowing your BMD gives you clear steps to protect your future mobility.
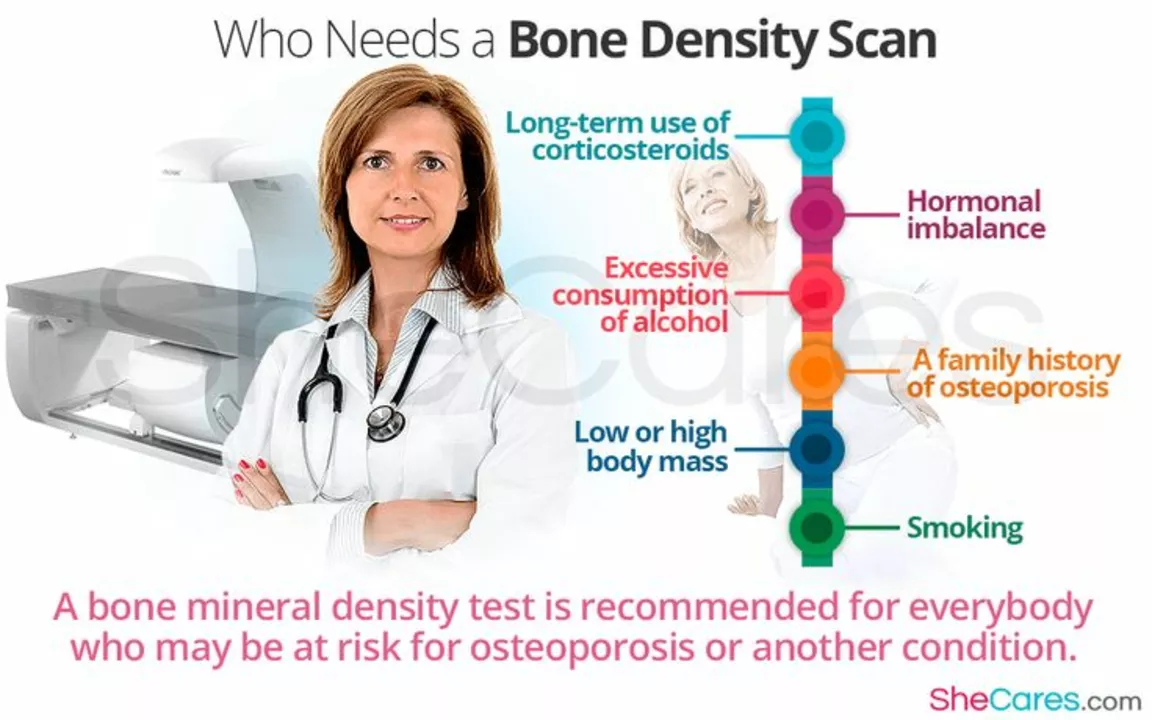
The standard test is a DEXA scan. It’s quick, painless, and reports a T-score: above −1 is normal, −1 to −2.5 is osteopenia, and −2.5 or lower is osteoporosis. Most doctors recommend a baseline DEXA for women at menopause and men at age 70, sooner if you have risk factors.
Risk factors are easy to check: past fractures, family history of hip fracture, long steroid use, low body weight, smoking, heavy alcohol use, and conditions like rheumatoid arthritis or early menopause. If any of those apply, mention them when you book a scan.
Simple tests and numbers
Besides DEXA, your doctor may order labs: serum 25‑hydroxyvitamin D, calcium, kidney function, and thyroid tests. Low vitamin D is common and reversible; target blood 25‑OH vitamin D above 30 ng/mL for most people. If your DEXA shows osteopenia, repeating the scan every 2 years is common; with osteoporosis or rapid bone loss, scans may be yearly.
How to strengthen bones — practical steps
Start with diet: aim for about 1,000 mg of calcium daily if you’re an adult under 50, and about 1,200 mg if you’re over 50. Get calcium from dairy, fortified plant milks, canned salmon with bones, or a supplement if needed. For vitamin D, many adults need 600–800 IU daily, but people with low levels often need higher replacement under doctor guidance.
Exercise matters. Do weight‑bearing activities like brisk walking, hiking, or dancing most days, and add resistance training two to three times weekly—think squats, lunges, and light weights. Include balance and mobility work—tai chi or single‑leg stands—to cut fall risk.
Medications exist when lifestyle changes aren’t enough. Bisphosphonates, denosumab, or calcitriol analogs can reduce fracture risk for people with osteoporosis. Discuss benefits and side effects with your clinician; treatment decisions use your BMD, age, and overall fracture risk.
Simple daily habits help too: stop smoking, limit alcohol to two drinks or less per day, secure loose rugs, and improve lighting at home. If you take steroids or other bone-impacting drugs, ask your doctor about bone protection early.
Want a fast next step? Check if you qualify for a DEXA, get vitamin D labs, and start two small routines today—a short daily walk and one resistance exercise. Small consistent moves add up to stronger bones over time.
If you start prescription bone drugs, plan for follow-up. Your doctor will check kidney function, calcium levels, and repeat DEXA at set intervals. Some drugs need drug holidays after several years — ask about long-term plans. Report new back pain or height loss quickly; those can signal vertebral fractures. Keep a list of your medicines and supplements to avoid interactions. Talk to a bone specialist.