Recently, I've been researching the effects of Bisoprolol Fumarate on the liver and I've discovered some interesting information. It seems that this medication, which is commonly used to treat high blood pressure and heart-related issues, is generally safe for liver health. In fact, it is metabolized by the liver and has a low risk of causing liver damage. However, it's always important to monitor liver function while taking any medication, so regular check-ups are crucial. If you have pre-existing liver issues, it's best to discuss with your doctor before starting Bisoprolol Fumarate to ensure your liver can handle the medication.
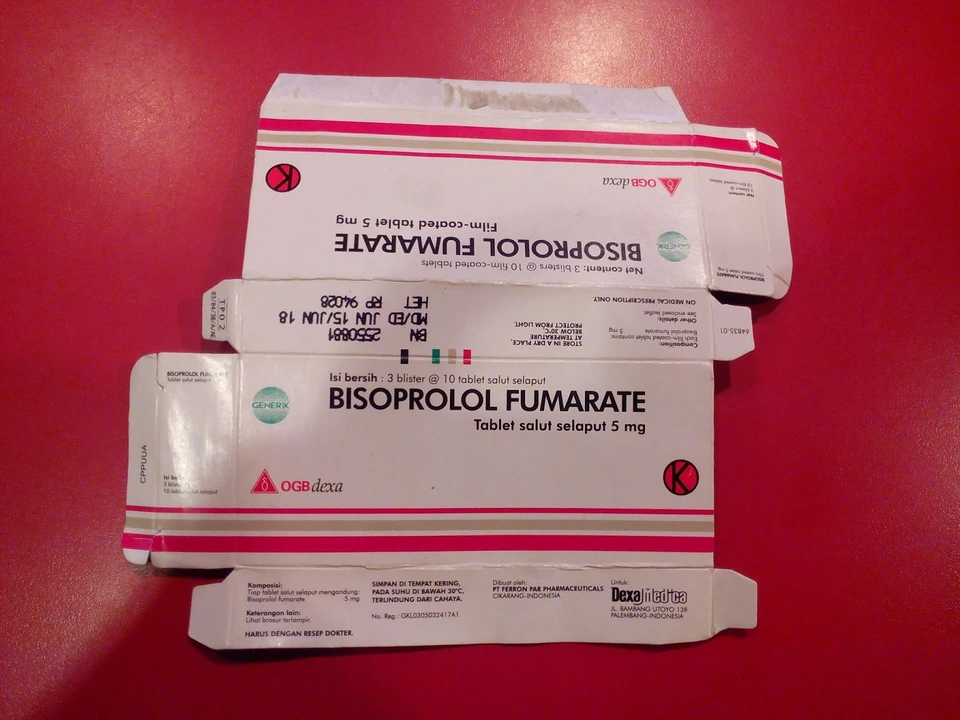
Bisoprolol fumarate: What it is and how to use it
Bisoprolol fumarate is a beta-blocker doctors prescribe for high blood pressure, certain kinds of chest pain (angina), and long-term heart failure care. It slows your heart rate and lowers blood pressure, which helps your heart work with less stress. The tablet is usually taken once a day, around the same time, with or without food.
How it works
Bisoprolol blocks beta receptors in the heart. That makes your heart beat slower and with less force. Slowing the heart lowers oxygen demand and often reduces symptoms like shortness of breath or chest tightness. For blood pressure, lower heart output and restricted adrenaline effects help bring numbers down.
Practical tips and dosing
Typical adult doses start at 5 mg once daily for high blood pressure, and many people move to 2.5–10 mg depending on response. For heart failure, doctors start lower and raise the dose slowly. Don’t change or stop the pill suddenly — stopping fast can cause worsening chest pain or rapid heart rate. Check your pulse regularly; if it’s under 50 beats per minute, call your doctor.
Watch for common side effects: tiredness, dizziness when standing, cold hands or feet, and mild stomach upset. More serious signs that need urgent care include fainting, severe shortness of breath, new swelling in the legs, or very slow pulse. If you have asthma or COPD and notice more wheeze, tell your prescriber right away — beta-blockers can tighten airways in some people.
Drug interactions matter. Combining bisoprolol with other drugs that lower heart rate or blood pressure — like certain calcium channel blockers (verapamil, diltiazem), digoxin, or some antiarrhythmics — can make your pulse very slow or cause dizziness. Alcohol and some herbal products can add to lightheadedness. If you take diabetes medicines, remember beta-blockers can hide signs of low blood sugar like a fast heartbeat; check glucose more often until you know how the drug affects you.
Adjustments may be needed with kidney or liver problems, so share your full medical history. Pregnant or breastfeeding? Talk to your doctor. They will weigh risks and benefits.
Practical checklist before starting bisoprolol fumarate: know your baseline blood pressure and pulse, learn when to seek help for side effects, avoid driving until you know how it affects you, and keep a list of other medicines and supplements to show your pharmacist or doctor. Carry a note of the drug name and dose in case of emergency.
If you have questions about how bisoprolol fits with other medicines or conditions, ask your prescriber. Small changes to dose and timing can make a big difference in safety and how well it works.
Monitoring and follow-up: Expect your doctor to check blood pressure and pulse a few weeks after starting. Lab tests aren't always needed but may be done if you have kidney problems. Keep a diary of readings and symptoms. If side effects are bothersome, many notice improvement after two to four weeks or call your doctor.