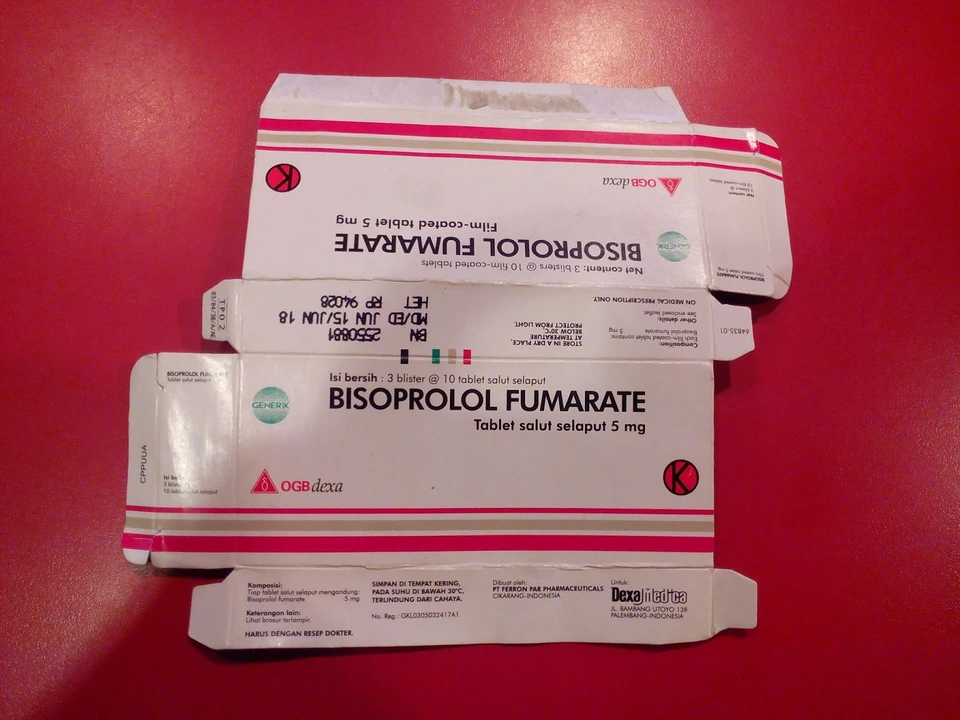
Recently, I've been researching the effects of Bisoprolol Fumarate on the liver and I've discovered some interesting information. It seems that this medication, which is commonly used to treat high blood pressure and heart-related issues, is generally safe for liver health. In fact, it is metabolized by the liver and has a low risk of causing liver damage. However, it's always important to monitor liver function while taking any medication, so regular check-ups are crucial. If you have pre-existing liver issues, it's best to discuss with your doctor before starting Bisoprolol Fumarate to ensure your liver can handle the medication.
Beta-blocker basics: what they do and why people take them
Beta-blockers are a group of medicines that slow your heart rate and lower blood pressure by blocking the body's "fight-or-flight" signals. That simple action helps with conditions like high blood pressure, certain arrhythmias, angina, heart failure, and even migraine prevention or essential tremor. Common names you’ll see are metoprolol, propranolol, atenolol, and carvedilol. They work fast for some problems, but they can cause side effects and need care when you stop taking them.
How they work and common uses
Think of beta receptors as switches that speed your heart up. Beta-blockers flip some of those switches off. Lower heart rate and contractility means less work for an overworked heart and lower blood pressure. Doctors prescribe them for: high blood pressure, heart rhythm problems (like atrial fibrillation), chest pain from reduced blood flow (angina), after a heart attack to protect the heart, and for preventing migraines or calming tremors. Different beta-blockers target receptors slightly differently—some are selective for the heart, others block more types of receptors, so the choice depends on the condition and side effects.
Safety tips, side effects, and drug interactions
Know the common side effects: tiredness, lightheadedness, cold hands or feet, slow pulse, and sometimes sleep changes or vivid dreams (propranolol often causes this). People with asthma or severe COPD may get worse breathing because beta-blockers can tighten airways—tell your doctor if you have any breathing condition. If you have diabetes, beta-blockers can hide the fast heartbeat that warns you of low blood sugar, so monitor glucose more closely.
Some drug interactions matter. Combining beta-blockers with calcium-channel blockers (like verapamil) can slow the heart too much. Diuretics such as furosemide are often used together for heart failure — that’s common and usually intentional, but your blood pressure and electrolytes need monitoring. Enzyme-inducing antibiotics like rifampin can lower levels of certain beta-blockers, reducing their effect. And never stop beta-blockers suddenly—taper off under a doctor’s plan or you risk rebound high blood pressure or chest pain.
Practical tips: check your pulse and blood pressure at home, take the drug at the same time each day, avoid driving or heavy machinery until you know how it affects you, and always tell healthcare providers and pharmacists about other medicines you use. If you’re buying meds online, choose a reputable pharmacy and confirm the product matches your prescription.
Questions for your prescriber: what are the target blood pressure and pulse numbers, how long should I take this, what symptoms should make me call right away, and how should we taper when it's time to stop? Getting clear answers up front makes the treatment safer and easier to live with.