In recent studies, I've discovered a fascinating connection between Alzheimer's Disease and vision loss. It appears that individuals with Alzheimer's often experience vision-related issues, such as difficulty recognizing faces and objects or perceiving depth. This could be due to the fact that Alzheimer's affects the brain's ability to process visual information, leading to impaired sight. As a result, it's important to closely monitor any changes in vision for those at risk of developing Alzheimer's. Early intervention and treatment may help slow the progression of both conditions, improving quality of life for those affected.
Alzheimer's disease: Practical help for symptoms, treatment, and care
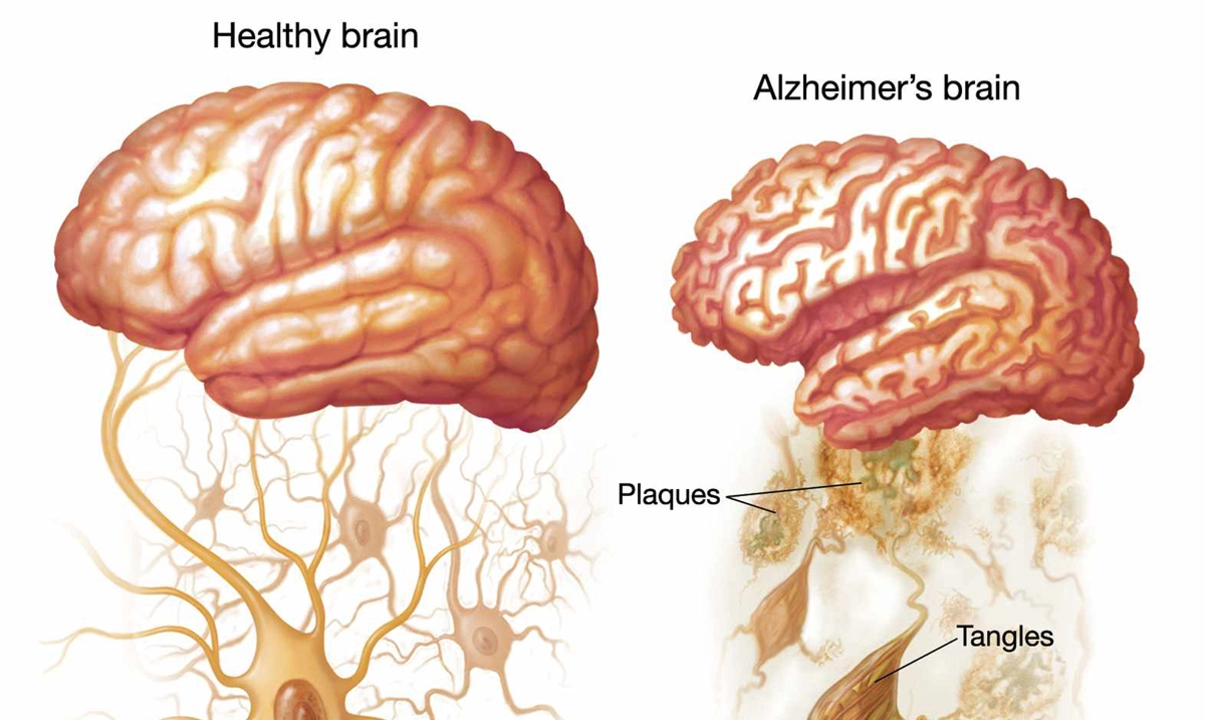
Alzheimer's disease is a progressive brain disorder that changes how a person thinks, remembers, and acts. Many people assume memory loss is normal aging, but Alzheimer's is different: it steadily erodes daily skills and personality. If someone you love shows repeated confusion, getting lost in familiar places, or sudden trouble managing money, those are red flags worth checking with a doctor.
Early diagnosis matters. Seeing a doctor sooner can slow decline with medications, lifestyle shifts, and planning. Standard drugs like cholinesterase inhibitors and memantine do not cure the disease, but they can ease symptoms and keep people independent longer. Ask your clinician about side effects, dosing, and what real-life improvements to expect.
Care strategies make daily life safer and calmer. Simple routines reduce anxiety: same wake-up time, clear labels on drawers, and one-step instructions work better than long explanations. Cut down clutter, improve lighting, and remove trip hazards. For meals, serve finger foods if utensils become hard to manage. These small changes lower stress for both the person with Alzheimer's and their caregiver.
Communication tips help when words fail. Use short sentences, yes/no questions, and slow speech. If memory slips, respond to the emotion rather than the facts: agree with the feeling, then redirect gently. For example, if someone worries about missing work decades ago, you might say, "That sounds stressful," then offer a calming activity like folding a towel together.
Caregiver support is crucial. Burnout is common, so ask for help early. Use adult day programs, hire respite care, or trade shifts with family. Legal and financial planning must start early too: set up power of attorney, review wills, and document medical wishes while the person can still decide.
Lifestyle moves that help brain health include regular physical activity, a Mediterranean-style diet, social engagement, and good sleep. These habits don't reverse Alzheimer’s but can reduce risk and slow decline. Some trials show aerobic exercise improves thinking skills modestly in early stages.
When behavior changes or wandering start, safety planning becomes central. Install door alarms, use ID bracelets, and keep a recent photo and list of medications handy. Discuss driving early; many with Alzheimer's should stop driving for safety. Work with clinicians and local support groups for tailored advice.
Clinical trials and research are active areas. New drugs aim to target underlying protein changes, and diagnostic tools are improving. If interested, ask your doctor about trials in your area—participation may offer access to new treatments and extra monitoring.
Finally, use trusted sources: national Alzheimer’s associations, memory clinics, and your primary doctor. Beware of miracle cures or unproven supplements. With the right planning, care, and support, families can maintain quality of life and dignity for longer.
Quick checklist for families
Get a medical evaluation, write down daily routine, simplify the home, discuss finances and legal plans, schedule regular exercise and social activities, join a caregiver support group, and ask about clinical trials. Keep a pill list and emergency contacts on the fridge.