Priority vs Standard Review: How FDA Prioritizes Generic Drug Applications
The U.S. Food and Drug Administration (FDA) doesn’t treat every generic drug application the same. Two paths exist: priority review and standard review. The difference isn’t just paperwork-it’s money, timing, and access to life-saving medications. For generic drug makers, getting priority review can mean launching a product months earlier, capturing market share before competitors, and generating hundreds of millions in revenue. For patients, it means faster access to affordable drugs, especially when there’s a shortage. But how does the FDA decide which applications get the faster track?
What’s the Difference Between Priority and Standard Review?
The FDA sets clear deadlines for each review type under the Generic Drug User Fee Amendments (GDUFA) III, which started in October 2022 and runs through 2027. Standard review takes up to 10 months from the date the application is officially accepted. Priority review cuts that time to 8 months. Sounds simple, right? But here’s the catch: only certain applications qualify for priority review. The rest automatically go to standard.Think of it like airport security. Standard review is the regular line. Priority review is TSA PreCheck. You don’t get to skip ahead unless you meet specific criteria. And those criteria are strict.
Who Gets Priority Review?
The FDA doesn’t hand out priority review like free samples. It’s reserved for three main types of applications:- First generics - The very first generic version of a brand-name drug after its patents and exclusivity expire. These are the most valuable because they get 180 days of market exclusivity, meaning no other generic can enter during that time. In 2022, 92.7% of first generics received this exclusivity.
- Drugs in shortage - If a drug is in short supply and patients are at risk, the FDA can fast-track any generic version to help fill the gap. This includes antibiotics, insulin, and other critical medicines.
- Medically important advances - Generic versions that offer real improvements over existing ones, like better stability, fewer side effects, or easier dosing. This category is rare but growing.
These aren’t vague categories. The FDA uses hard data to make the call. For example, if a drug appears on the FDA’s official Drug Shortage List, that alone can trigger priority review. The agency tracks these shortages in real time and responds quickly.
The New Domestic Manufacturing Pilot
In October 2023, the FDA added a new twist: the ANDA Prioritization Pilot Program. This isn’t just about speed anymore-it’s about security. The goal? To bring more generic drug manufacturing back to the United States.To qualify for priority review under this pilot, a company must prove three things:
- The bioequivalence studies were done in the U.S.
- The finished drug is made in a U.S. facility.
- The active ingredient (API) comes from a U.S.-based supplier.
Why does this matter? In 2021, the FDA reported that 80% of active ingredients for all drugs-brand and generic-were made outside the U.S. That became a huge problem during the pandemic. When supply chains broke, shortages spiked. This pilot is the FDA’s way of forcing companies to build resilience into their supply chains.
But here’s the reality: only 12.3% of generic drug companies currently meet all three criteria. That’s not because they don’t want to. It’s because sourcing U.S.-made APIs and manufacturing facilities for complex drugs is expensive and hard. Many rely on suppliers in India and China because they’ve been doing it for decades.
Why Does This Matter for Patients and Prices?
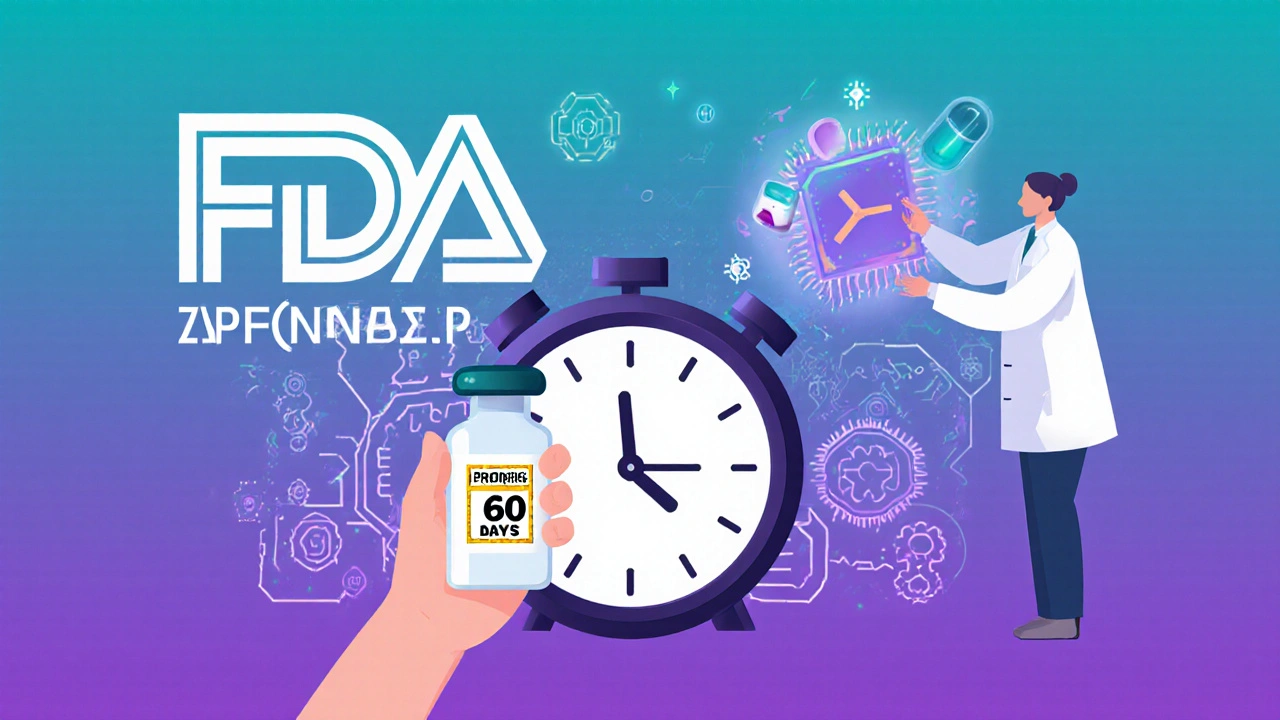
Generic drugs make up 88.6% of all prescriptions filled in the U.S., but only 15.3% of total drug spending. That’s how they save money. When a first generic hits the market, prices for that drug can drop by 70-90% within months. If the FDA approves that generic 2 months earlier, patients get those savings sooner.For example, a cardiovascular drug that costs $300 per month as a brand-name pill might drop to $15 after the first generic launches. If that generic gets priority review, thousands of patients get access to that $15 version two months earlier than they otherwise would. That’s thousands of dollars saved per patient in just 60 days.
And it’s not just about cost. When a drug is in short supply, patients may go without. Priority review can mean the difference between getting your insulin on time or going without for weeks.
What Happens When an Application Gets Rejected?
Even if you submit a complete application, it doesn’t mean approval is guaranteed. In 2022, 31.7% of original ANDAs got a Complete Response Letter (CRL)-basically, a “not quite” notice. The most common reason? Problems with chemistry, manufacturing, or controls (CMC). That’s a fancy way of saying the drug wasn’t made consistently enough to be safe.Each CRL adds about 4.2 months to the review clock. And most applications need 1.7 review cycles before they’re approved. That means even if you start with priority review, you could end up with a 12-month timeline if you get stuck in revisions.
That’s why more companies are using the FDA’s pre-submission meetings. In 2020, only 41% of sponsors had these meetings. By 2023, that number jumped to 63%. These meetings let companies ask the FDA, “Will this work?” before spending hundreds of thousands on testing. It’s not free-it costs time and money-but it cuts down on costly rejections.
What’s Changing in 2024 and Beyond?
The FDA isn’t standing still. In 2023, they launched a pilot program to help with complex generics-things like inhalers, topical creams, and extended-release pills. These are harder to copy because the way the drug is delivered matters as much as the chemical itself. Right now, only 9.7% of these complex generics get approved, even though they make up nearly 20% of pending applications.And in Q3 2024, the FDA plans to roll out AI tools to help speed up reviews for simpler applications. In internal tests, AI reduced review times by 18.7%. That might not sound like much, but for a company waiting to launch, even a few weeks matters.
By 2026, analysts estimate these changes could cut the average time to generic approval by 4.3 months. That could save the U.S. healthcare system $18.7 billion a year.
Industry Reactions: Real Voices
Not everyone is thrilled. On Reddit, a senior regulatory affairs manager wrote: “The domestic manufacturing requirement is noble but unrealistic for complex generics where 92% of specialized excipients still come from Europe and Asia.”But another voice on the same thread said: “We’ve already shifted two product lines to our Pennsylvania facility. The 2-month review acceleration could mean $120M in additional revenue for our key cardiovascular product.”
That’s the split. Some see the new rules as a barrier. Others see them as a competitive edge.
Big players like Teva, Sandoz, and Hikma are already investing in U.S.-based bioequivalence labs. Contract research firms like Covance and PPD are reporting 35% growth in U.S. testing capacity year-over-year. The race is on.
What Should Generic Drug Companies Do Now?
If you’re applying for FDA approval, here’s what you need to do:- Check if your drug qualifies as a first generic or is on the shortage list. If yes, aim for priority review.
- If you’re not sure, talk to the FDA early. Use the pre-submission meeting program.
- Start mapping your supply chain. Can you source your API from the U.S.? Do you have a U.S. manufacturing site? If not, plan for it now.
- Don’t assume your application is ready. CMC issues are the #1 reason for delays. Test, test, test.
The FDA isn’t trying to make things harder. It’s trying to make the system more reliable-for patients, for manufacturers, and for the country’s health security. The rules have changed. The clock is ticking. And the next generic drug to hit the market? It might be yours-if you play the game right.
What is the difference between priority review and standard review for generic drugs?
Priority review takes 8 months from submission, while standard review takes 10 months. Priority review is only given to applications that meet specific criteria: first generic versions of brand-name drugs, drugs in shortage, or those offering a meaningful medical improvement. Standard review applies to all other generic applications.
How do I know if my generic drug qualifies for priority review?
Your application qualifies for priority review if it’s the first generic version of a brand-name drug after its patents expire, if the drug is on the FDA’s official shortage list, or if it offers a significant medical advantage over existing generics. You must submit evidence to support your claim, and the FDA evaluates it during the initial filing review.
What is the ANDA Prioritization Pilot Program?
The ANDA Prioritization Pilot Program, launched in October 2023, gives priority review status to generic drug applications that use U.S.-manufactured active ingredients, U.S.-based finished drug manufacturing, and U.S.-conducted bioequivalence testing. It’s designed to strengthen domestic supply chains and reduce reliance on foreign manufacturing.
Why are so many generic drug applications rejected?
About 32% of applications receive a Complete Response Letter (CRL), mostly due to issues with chemistry, manufacturing, and controls (CMC). This means the drug wasn’t produced consistently enough to meet safety and quality standards. Many companies now use pre-submission meetings with the FDA to avoid these problems before filing.
Can a generic drug get priority review even if it’s not the first one on the market?
Yes, but only if the drug is in shortage or offers a medically important improvement over existing generics. First generics automatically qualify. Other generics can qualify only if they address a critical public health need, such as a drug with no available alternative or one with better safety or dosing features.
How has the FDA improved the approval process since 2022?
Since 2022, the FDA has launched the ANDA Prioritization Pilot, expanded pre-submission meetings, created a Complex Generic Drug Product Pilot for difficult-to-copy drugs, and is testing AI tools to speed up reviews. These changes have increased the number of priority reviews and improved approval rates for complex products.

Pallab Dasgupta
Bro, this is wild - 80% of APIs come from India and China, and now the FDA wants us to make everything in the US? 😅 I get the patriotism, but let’s be real - we don’t have the infrastructure for complex APIs yet. We export generics, we don’t make them. This feels like forcing a Ferrari to run on bicycle tires.
Erika Hunt
Okay, I’ll admit - I didn’t realize how much of a bottleneck CMC issues were. I thought it was just paperwork… but no, it’s literally about whether the drug was mixed in a way that won’t kill someone. I mean, if the particle size is off by 5 microns, the body absorbs it wrong. That’s not a typo - that’s a life-or-death margin. And yet, 31.7% get rejected? That’s insane. We need more labs, more inspectors, more training - not just more slogans about ‘American-made.’
Jennifer Griffith
so like… if i make a generic in india and ship it here, its automatically standard review? lol ok
Ellen Sales
There’s a quiet revolution happening here - not in boardrooms, but in clean rooms. The companies that are shifting production to Pennsylvania, Ohio, North Carolina? They’re not doing it for the FDA’s approval. They’re doing it because they realized that global supply chains are just… fragile. Pandemics, wars, port strikes - none of that matters if your API comes from a lab 10 miles from your factory. This isn’t nationalism. It’s common sense. And yes, it’s expensive. But so is a patient dying because their insulin was delayed by a shipping container stuck in the Suez.
Andrew Camacho
Oh great. Another ‘patriotic’ regulation that only helps big pharma. Small companies? Forget it. You think a startup can afford a U.S.-made API? Nah. They’ll get crushed. And the FDA? They’re just playing politics. Meanwhile, patients are still waiting. This isn’t innovation - it’s bureaucratic theater. We’re turning healthcare into a patriotism contest. And guess who pays? The people who can’t afford the $15 insulin - because the $15 version never got approved.
Arup Kuri
They’re using this pilot to control the market. First they make it impossible for foreign manufacturers to compete. Then they let their buddies in the U.S. monopolize the supply. It’s not about safety - it’s about profit. Look at who owns the new U.S. labs - same names that run the brand-name drugs. This isn’t a public health move. It’s a corporate takeover. And they’re calling it ‘security’? Please.
Elise Lakey
I just want to know - how many patients actually benefit from a 2-month faster approval? Is it just a few hundred? Or thousands? I feel like the narrative skips over the human scale. If a drug saves 10 people a month, is that worth the cost of rebuilding an entire supply chain? Or is this more about symbolic victory than measurable impact?
prasad gaude
From India, I see this every day. We make the APIs. We test them. We ship them. And now you want us to stop? I respect the goal - domestic supply chains are important. But you can’t just flip a switch. It takes decades to build trust, capacity, and expertise. Maybe instead of forcing us out, you could partner with us? Train your workers here. Invest in joint labs. We’re not the enemy. We’re the backbone of your generic market.
Timothy Sadleir
It is imperative to note that the foundational premise of this regulatory evolution is predicated upon the strategic imperative of national biosecurity. The reliance upon foreign-sourced active pharmaceutical ingredients constitutes a critical vulnerability in the United States’ healthcare infrastructure. The ANDA Prioritization Pilot Program is not merely a procedural adjustment - it is a sovereign recalibration. One must recognize that the erosion of domestic manufacturing capability is a direct consequence of decades of neoliberal economic policy, which prioritized cost-efficiency over resilience. This is not a burden - it is a necessary reclamation.
Roscoe Howard
Let’s be honest - this whole system is rigged. The FDA lets Indian and Chinese companies flood the market with cheap generics, then when they finally get around to fixing it, they slap a ‘Made in America’ sticker on it and call it ‘patriotic.’ Meanwhile, real American workers are getting laid off while CEOs buy yachts. This isn’t about patients. It’s about making Americans feel better about paying more. And don’t even get me started on the AI tools - they’re just a fancy way to cut jobs. 🇺🇸
Shirou Spade
There’s a deeper tension here - between efficiency and sovereignty. We’ve spent 30 years optimizing for cost, and now we’re realizing that optimization isn’t the same as sustainability. The FDA isn’t being punitive - they’re being prophetic. The next crisis won’t be a pandemic. It’ll be a cyberattack on a single API plant in Gujarat. And then we’ll have no insulin for 3 months. This pilot? It’s insurance. Expensive insurance. But insurance nonetheless.
Lisa Odence
AI reducing review time by 18.7%? That’s HUGE. 🤖💖 Imagine if this tech could also flag CMC issues before submission - like a spellcheck for drug manufacturing. The FDA needs to open this up to third-party developers. And yes, I know some people are scared of AI… but if it means my grandma gets her blood pressure med on time, I’m all in. 🌟 Let’s not overthink this - speed + safety = win. #FutureOfPharma
Jefriady Dahri
My uncle works in a U.S. lab that does bioequivalence testing. He said they’re hiring 3x as many people since 2023. This isn’t just policy - it’s jobs. Real jobs. With benefits. In places that got left behind. I used to think generics were just ‘cheap pills.’ Now I see it: they’re the heartbeat of American healthcare. And yeah, it’s messy. It’s expensive. But it’s worth it. 🙌