Opioid-induced constipation affects up to 60% of patients on long-term pain meds. Learn how to prevent it from day one and when to move beyond laxatives to prescription treatments like PAMORAs.
Opioid Side Effects: What You Need to Know Before Taking Them
When you take opioids, a class of pain-relieving drugs that work on the brain’s reward and pain centers. Also known as narcotics, they’re prescribed for severe pain but carry risks that many patients don’t fully understand. These drugs don’t just numb pain—they change how your brain and body function, and that’s where the side effects start.
One of the most dangerous opioid side effects, a set of physical and psychological reactions caused by opioid use is respiratory depression, slowed or stopped breathing due to opioid overdose. It’s not rare. In fact, it’s the leading cause of death in opioid overdoses. You might not feel it coming—no burning sensation, no warning crash. Just slower breaths, then silence. That’s why doctors adjust doses carefully, especially for people with kidney problems, as seen in posts about opioid dosing CKD and safe choices like fentanyl or buprenorphine for those with reduced kidney function.
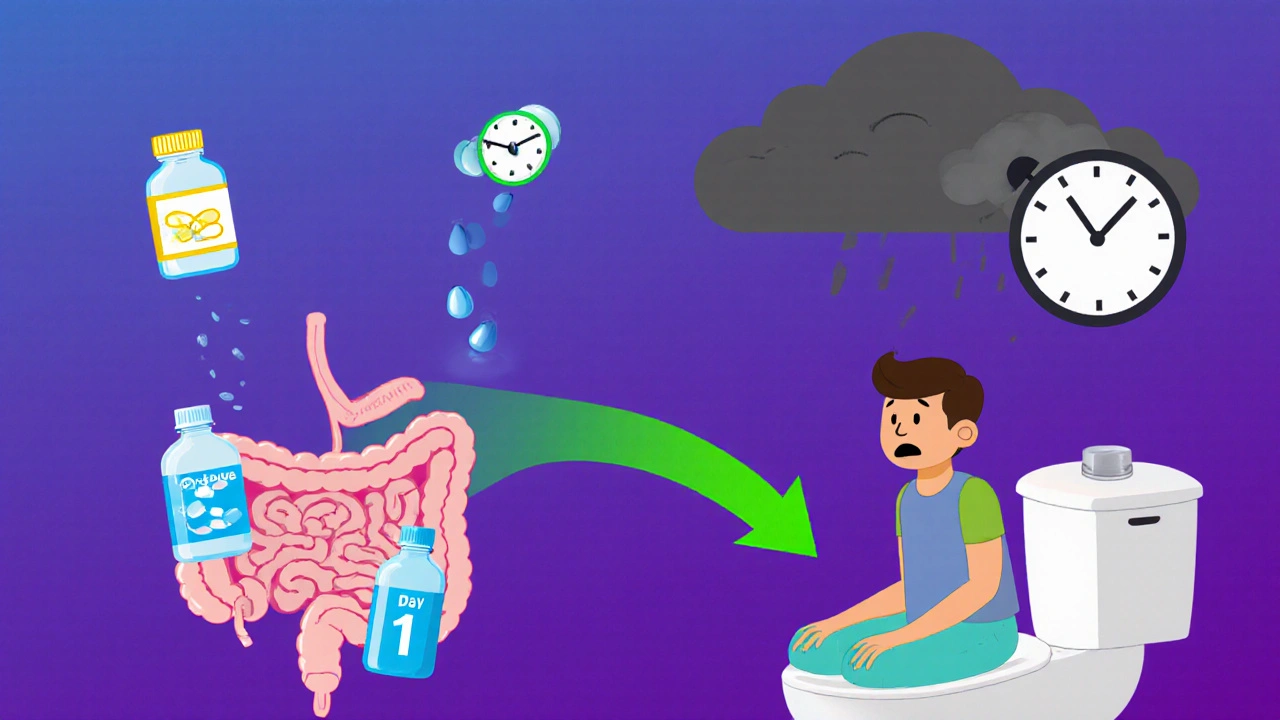
Then there’s constipation from opioids, a near-universal side effect caused by slowed digestion. It’s not just uncomfortable—it can lead to bowel obstructions if ignored. Unlike nausea or drowsiness, which often fade after a few days, constipation sticks around as long as you’re on the drug. That’s why many guides, like those on opioid side effects, stress combining opioids with stool softeners or laxatives from day one.
Dependence is another silent risk. Your body adapts. You need more to get the same relief. Stop suddenly, and withdrawal hits—sweating, shaking, nausea, insomnia. It’s not weakness. It’s biology. That’s why tapering under medical supervision matters, and why some patients switch to longer-acting opioids like buprenorphine to reduce cravings and stabilize their system.
And let’s not forget the mental side effects: mood swings, confusion, even depression. These aren’t just "bad days." They’re direct results of opioids altering brain chemistry. People on long-term therapy often feel emotionally flat, disconnected. It’s not all in their head—it’s in their neurons.
What you’ll find in the posts below isn’t just a list of symptoms. It’s real-world guidance: how to spot early signs of trouble, how to talk to your doctor about safer options, how to manage side effects without quitting pain relief altogether. From kidney patients needing adjusted doses to those worried about addiction, the advice here is practical, tested, and focused on keeping you safe—not just numb.